José de Jesús Curiel-Valdés MD1*+, José de Jesús Macias-Duvignau MD2, Roberto Manriquez-Angulo MD2, Gabriel Rufino Merchan-Escalante MD3, Alfredo Saad Ganem MD++, Rubi Azeneth Baca Patiño MD+, Wilson Toscano-Renfigo MD+, Jesús Cienfuegos-Meza MD4, Verónica del Rocio Lliguisupa Pelaez MD1, Torres Cunalata KL MD1
1Academia Mexicana de Cirugía, Laboratorio Grupo Diagnóstico
+Laboratorio Grupo Diagnóstico
2Ginecólogo Hospital San Ángel Inn Chapultepec
3Ginecólogo Centro Médico Dalinde
4Instituto Nacional de Neurología y Neurocirugía.
++Ginecólogo Hospital Español
*Corresponding Author: José de Jesús Curiel-Valdés MD, Academia Mexicana de Cirugía, Laboratorio Grupo Diagnóstico.
Abstract
Background: Abnormal uterine bleeding (AUB) is quite common, one third of women have it and there are women in whom no cause is detected that explains it. To date no reported histological findings that justify the bleeding are published.
Objective: To describe the hitherto unknown cause of AUB, which consists of markedly abnormal vessels in the endo myometrial junction of the uterus (EMJ) that we call Uterine Vascular Hyperplasia (UVH).
Method: 520 uteri were reviewed between October 2022 and August 2024, 39 without macroscopic alteration that justified the AUB. Characteristically they have more than 3 vessels in balls in the EMJ, where the number of vessels, outer diameter, thickness of the vessel wall and diameter of the lumen were evaluated. The control group (CG) of 39 uteri from cases without UAB.
Results: All cases with UAB had abnormal vessels in average number of 12.2 VS 3.0 CG, external diameter: 187 microns ((μm) with UAB VS 24.9μm in the CG, the vessel lumen: 71.3μm UAB VS 13.0 μm of the CG, wall thickness: 57.9μm UAB VS 5.9μm CG, with p= <0.0001 in all parameters.
Conclusion: It is described for the first time the finding of abnormal vessels as a possible origin of idiopathic or unknown cause of UAB that consists of the presence of abnormal ball vessels with an increase in the quantity, size of the external diameter, wall thickness and diameter of the lumen that compared with normal CG is between 4 to 9.8 times greater, which explains the UAB.
Keywords: Uterine Bleeding. Abnormal uterine Bleeding. PALM-COEIN. Unknown uterine bleeding.
Introduction
Background
Uterine abnormal bleeding (UAB) is common, approximately one third of women worldwide have it in their reproductive age, the reported worldwide prevalence of is between 3% and 52% [1,2,3,4,5]. Nine main categories of UAB are defined and are summarized in the acronym PALM-COEIN and each letter indicates a cause: PALM: Polyp, Adenomyosis, Leiomyoma (uterine fibroids), Malignant neoplasia, COEIN: Coagulopathy, Ovulatory dysfunction, Altered endometrium, Iatrogenic (intrauterine devices, surgical procedures, etc.) and other unknown causes [2]. The reason for this study is that a small group of UAB does not have a detectable anatomical or functional cause, which falls into the group of unknown causes (UABUC). These women have hypermenorrhea or metrorrhagia, which is defined as very heavy bleeding during menstruation that exceeds 80 ml per cycle, and many have significant anemia, leading one-third of them to undergo hysterectomy due to uncontrollable bleeding [6]. There are many articles that comment on the clinical aspects and compare methods to correct them [4, 5, 7, 8]; however, we did not detect any report that mentions the histological findings in uteri that are removed for AUBUC, either in publication in journals or as content in gynecological pathology textbooks [9-12].
The first case where the abnormality described was detected was that of my daughter with a history of UAB, uncontrollable hypermenorrhea for more than 7 years, and secondary anemia. Treatments with hormones and other medications had no effect. A hysterectomy was performed; the diagnosis initially made in the hospital's pathology department did not show any alteration that would explain the bleeding, so the uterus was thoroughly examined. The original sections were examined and additional serial sections of the anterior and posterior wall were also performed, finding a large number of thick arterial vessels in balls at the endo- myometrium junction (EMY) in a diffuse manner, as well as an increase in the number and thickness of arterial vessels throughout the thickness of the myometrium. Normally the radial arteries of the myometrium are of large caliber and tortuousness in the external third of the myometrium, they are branches of the right and left uterine arteries that become thinner as they penetrate the middle and internal third and towards the endometrium in a horizontal and vertical manner that when they penetrate the endometrium are already small arteries called spirals [6-10]. Middlelkoop [7] in a thorough review of 35 publications of cases with normal and abnormal uterine bleeding, found that in UAB there is an increase in the diameter of the spiral arteries in the endometrium that conditions bleeding due to high pressure and increased flow due to the increased diameter of the spiral arteries compared to the diameter of cases without abnormal bleeding, all of these publications analyze the findings in the endometrium and none of them analyze the EMY or the immediate area of the myometrium. However, in books and articles on pathology, this vascular alteration in the endometrium or in hysterectomies is not mentioned [9-12].
The objective of this work is to describe for the first time the in the literature the abnormal increase in the number of vessels with a larger diameter and arranged in balls at the EMY and the adjacent area of the myometrium and which we call Uterine Vascular Hyperplasia (UVH).
Material and methods
520 uteri (100%) received for study consecutively for any reason between October 2022 and August 2024 were prospectively reviewed. 39 cases (7.5%) were detected that did not macroscopically show any alteration such as leiomyomas, adenomyosis, polyps, hyperplasia or endometrial neoplasia that justified the AUB. The clinical data of the 39 patients were obtained from the request received with the tissue and the missing data were completed through direct communication with the surgeon, mainly age, reason for surgery, presence or absence of anemia and whether or not there was abnormal uterine bleeding. Two wide cuts of the anterior and posterior wall, total 4 areas of the uterine body were made (in addition to the usual routine cuts of the rest of the uterus) including the endometrium and the entire thickness of the myometrium up to the serosa. The search for the vessels was conducted at the EMY, with a 10X lens, placing the edge of the endometrium at one end of the field and the myometrium at the other end, (Figure 1). Sites with three or more vessels were searched for and called a ball, the number of vessels per ball was quantified, (Figure 1-2) and the dimension of the affected area in the four cuts of each case, considering the largest vessel for evaluation. The histological parameters to be considered in the balls were the following: Three or more arterial vessels, and in the largest one, external diameter, wall thickness and diameter of the lumen were measured, the measurement was made in microns with a NIKONR micrometer. The endometrial tissue was evaluated and did not show any abnormality that justified bleeding such as hyperplasia, polyps or adenocarcinoma and in the myometrium leiomyomas of any size including small submucosal ones, or adenomyosis not detected macroscopically. As a control group, a comparison was made in 39 uteri without AUB resected for other causes such as cervical dysplasia or carcinoma, ovarian tumors among others, in the same time period. The data were analyzed with the Stata v12 program (College Station, TX) and Prism v9 (GraphPad Software Inc. Descriptive statistics and Student's t-test were used to compare the difference between groups in relation to the mean number of vessels per ball, vessel diameter, vascular lumen diameter and vascular wall thickness. A p-value <0.05 was considered statistically significant.
All applications complied with the authorization to proceed with the study and use of the report and data submitted for research and publication purposes. The personal data of the patients were kept anonymous. The work was approved by an ethics committee.
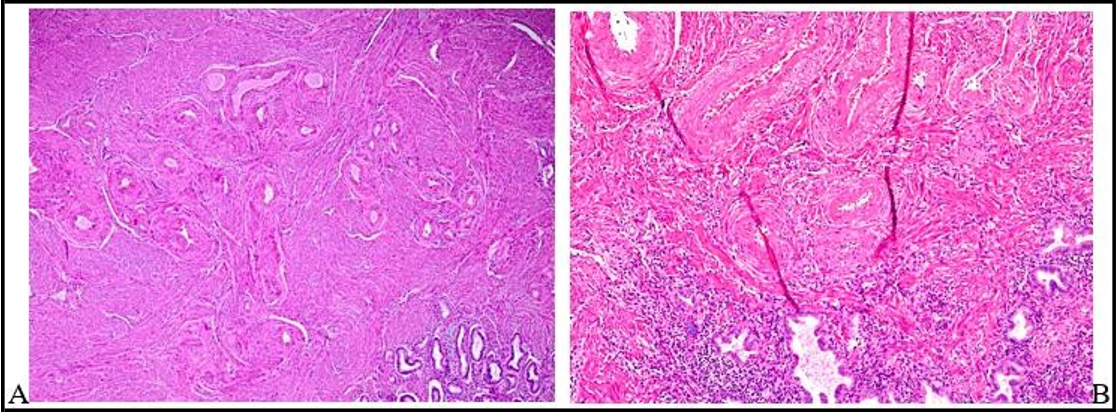
Figure 1: Panoramic in A and B of the endomyometrium junction, in A the endometrium is in the lower right part and in B in the entire lower part, A in 4X and B 10X. In both with UVH, in A 26 vessels, in B 8 vessels.
Figure 2: In A-D in 10X panoramic view, balls with large diameter vessels and thick walls. In A, C and D you can see the vessels with a wall thicker than their lumen and in B the wall is thick and the lumen wide.
Figure 3: A-D in detail 40X, vessels increased in number and large outer diameter, with thick walls, in C the vessels with walls thicker than their lumen. In A, B and D the wall is less thick and the lumen wide.
Figure 4: A: Basal layer of the endometrium 10X, with ball of abnormal vessels in number and diameter, as well as a wide lumen. B 10X also balls with abundant thick vessels and wide lumen that penetrate the inner third of endometrium. C: Compare with normal vessels in number and diameter of a case without UAB.
Figure 5: A and B Normal vessels in the EMY, they are small in external diameter and in their lumen, there are only 3 vessels per ball. Compare diameters with Figures 1 to 3
Results
The 39 cases, had an average age of 40.3 years, (28 to 52 years), all patients had UAB, between 6 months to 5 years, table 3, with an average of 2.5 years. All showed anemia that could be well documented in 15 of them, with Hb values between 6 and 10 g. Table 3. In the microscopic study, between 2 and 9 balls of vessels were found with average 3.1 vessel per ball. There were an average of 12.2 balls in the 4 sections (minimum 2, maximum 30) (Figures 3, 4) that covered an area of 1.46 mm in the 4 sections. In each ball there were between 3 to 30 vessels with an average of 12.2. The measurements of the largest diameter vessel evaluated in each case were: external diameter 187 microns (μm) with AUB VS 24.9μm, of CG, the vessel lumen: 71.3μm UAB VS 13.0 μm of CG, wall thickness: 57.9μm, AUB VS 5.9μm, of CG with p-value = <0.001, see table 1, finding a notable increase in all these parameters compared to normal cases (Figure 5), summarized in Table 2. In 27 cases (69.2%) the vessels entered the endometrium, and, in the rest, they were at the EMY.
Table 1: Characteristics Of Endomiometrial Blood Vessels In Hvu Cases
|
Case |
Vassels Per-Ball |
Vessel External Diameter Μm |
Vessel Lumen Diameter Μm |
Vessel Wall Thickness Μm |
|
N1 |
2 |
60 |
38 |
11 |
|
N2 |
3 |
22 |
13 |
4.5 |
|
N3 |
5 |
24 |
16 |
4 |
|
N4 |
3 |
18 |
9 |
4.5 |
|
N5 |
1 |
24 |
12 |
6 |
|
N6 |
3 |
18 |
8 |
5 |
|
N7 |
12 |
24 |
14 |
5 |
|
N8 |
1 |
36 |
24 |
6 |
|
N9 |
1 |
25 |
13 |
6 |
|
N10 |
3 |
12 |
4 |
4 |
|
N11 |
4 |
12 |
3 |
4.5 |
|
N12 |
1 |
29 |
17 |
6 |
|
N13 |
1 |
8 |
2 |
3 |
|
N14 |
2 |
36 |
9 |
13 |
|
HV1 |
15 |
130 |
45 |
42 |
|
HV2 |
15 |
280 |
16 |
132 |
|
HV3 |
16 |
480 |
230 |
125 |
|
HV4 |
23 |
168 |
72 |
48 |
|
HV5 |
22 |
108 |
32 |
38 |
|
HV6 |
16 |
120 |
48 |
36 |
|
HV7 |
9 |
216 |
72 |
72 |
|
HV8 |
12 |
132 |
70 |
31 |
|
HV9 |
11 |
136 |
26 |
55 |
|
HV10 |
5 |
192 |
48 |
72 |
|
HV11 |
12 |
194 |
26 |
84 |
|
HV12 |
15 |
211 |
121 |
45 |
|
HV13 |
10 |
192 |
96 |
48 |
|
HV14 |
6 |
72 |
36 |
24 |
|
HV15 |
6 |
136 |
36 |
38 |
|
HV16 |
5 |
156 |
28 |
64 |
|
HV17 |
5 |
194 |
18 |
88 |
|
HV18 |
5 |
153 |
73 |
40 |
|
HV19 |
14 |
172 |
24 |
74 |
|
HV20 |
30 |
260 |
66 |
97 |
|
HV21 |
4 |
120 |
94 |
13 |
|
HV22 |
20 |
204 |
94 |
35 |
|
HV23 |
12 |
144 |
20 |
62 |
|
HV24 |
5 |
228 |
108 |
60 |
|
HV25 |
10 |
336 |
16 |
160 |
|
HV26 |
18 |
144 |
48 |
48 |
|
HV27 |
17 |
150 |
40 |
55 |
|
HV28 |
11 |
145 |
73 |
36 |
|
HV29 |
22 |
110 |
62 |
24 |
|
HV30 |
8 |
205 |
25 |
90 |
|
HV31 |
12 |
136 |
40 |
48 |
|
HV32 |
23 |
168 |
64 |
52 |
|
HV33 |
5 |
124 |
52 |
36 |
|
HV34 |
16 |
124 |
66 |
29 |
|
HV35 |
9 |
180 |
116 |
32 |
|
HV36 |
7 |
220 |
60 |
80 |
|
HV37 |
8 |
225 |
95 |
65 |
|
HV38 |
9 |
350 |
260 |
45 |
|
HV39 |
8 |
300 |
265 |
35 |
|
N= Control Group; UVH= Uterine vascular Hiperplasia vascular |
||||
Table 2: Comparison between groups by blood vessel characteristics.
|
Group |
|
Vessel external diameter μm |
Vessel lumen diameter μm |
Vessel wall thickness μm |
|
Control (n=14) |
3.0 |
24.9 |
13.0 |
5.9 |
|
Hiperplasia (n=39) |
12.2 |
187.6 |
71.3 |
57.9 |
|
Valor p* |
<0.0001A |
<0.0001B |
0.0007C |
<0.0001D |
|
*t Student tes non paired : A) t (51) =5.2481, p<0.0001; B) t (51) =7.6722, p<0.0001; C) t (51) =3.5921, p=0.0007 ; D) t (51) =6.1894, p<0.0001. |
||||
Table 3: Clinical data
|
Case number |
Age |
UAB |
Evolution time years |
Anemia g/dl * |
|
1 |
28 |
Yes |
3 |
Yes |
|
2 |
45 |
Yes |
5 |
9 |
|
3 |
38 |
Yes |
3 |
8.8 |
|
4 |
42 |
Yes |
2 |
Yes |
|
5 |
29 |
Yes |
3 |
Yes |
|
6 |
32 |
Yes |
1 |
Yes |
|
7 |
44 |
Yes |
3 |
10 |
|
8 |
45 |
Yes |
1.5 |
Yes |
|
9 |
42 |
Yes |
2 |
11 |
|
10 |
38 |
Yes |
1 |
8 |
|
11 |
35 |
Yes |
2 |
10 |
|
12 |
42 |
Yes |
1 |
9 |
|
13 |
41 |
Yes |
2 |
9 |
|
14 |
40 |
Yes |
3 |
8.5 |
|
15 |
43 |
Yes |
1.5 |
Yes |
|
16 |
42 |
Yes |
2 |
10 |
|
17 |
35 |
Yes |
3 |
Yes |
|
18 |
37 |
Yes |
2 |
10 |
|
19 |
41 |
Yes |
2 |
Yes |
|
20 |
49 |
Yes |
0.5 |
Yes |
|
21 |
35 |
Yes |
0.5 |
Yes |
|
22 |
41 |
Yes |
1 |
Yes |
|
23 |
46 |
Yes |
1 |
Yes |
|
24 |
42 |
Yes |
2 |
Yes |
|
25 |
46 |
Yes |
3 |
Yes |
|
26 |
52 |
Yes |
1 |
Yes |
|
27 |
48 |
Yes |
2 |
Yes |
|
28 |
40 |
Yes |
3 |
Yes |
|
29 |
43 |
Yes |
3 |
Yes |
|
30 |
42 |
Yes |
4 |
Yes |
|
31 |
37 |
Yes |
3 |
Yes |
|
32 |
41 |
Yes |
2 |
Yes |
|
33 |
43 |
Yes |
3 |
9 |
|
34 |
30 |
Yes |
2 |
Yes |
|
35 |
42 |
Yes |
2 |
Yes |
|
36 |
47 |
Yes |
1 |
Yes |
|
37 |
43 |
Yes |
3 |
6 |
|
38 |
36 |
Yes |
1 |
Yes |
|
39 |
35 |
Yes |
3 |
Yes |
|
Average |
40.3 |
|
2.5 |
|
* Data mentioned without precise Hg measure.
Discussion
During menstruation, hormones are those that regulate the cycle, estrogens creating the proliferative phase and progesterone the secretory phase, the proliferation of spiral vessels that nourish the endometrium are small and barely visible in the proliferative phase and are thicker and in greater number in the secretory phase. When the action of progesterone in the spiral arteries ceases, blood flow decreases, causing menstruation due to a set of widely described physiological events [6] with detachment of the superficial layers, leaving the basal layer. Bleeding stops due to constriction of the arteries with thrombosis and by the action of the estrogens of the new cycle [6].
Middelkoop in 2023 [7] in a thorough systematic review of the literature on the causes of AUB in the endometrium of women with and without abnormal bleeding found that in cases with UAB the average diameter of the spiral arteries is 9.3 microns compared to 3.6 microns in endometrium's of women without abnormal bleeding and the diameter of the lumen is also larger, 2.7 microns VS 1.2 microns with UAB, they also find the endothelial cell layer incomplete, compared to women without abnormal bleeding. The results of the increased diameter showed that the flow was much higher in women with AUB that did not allow vasoconstriction, thus explaining the metrorrhagia. In this review, several angiogenesis factors are analyzed and found some contradictory results on their correlation with the number of vessels and their diameter. This review was only in endometrium samples, so the EMY vessels were not studied. The results in our cases show (Table 1) number of vessels per ball 12.2, average vessel diameter is 187.6 microns, the vessel lumen 71.3 microns and the vessel wall thickness 57.9 microns, comparing the same data in controls without SUA with less than 3 vessels, external diameter of the vessel in microns was 24.9, vessel lumen 13 and vessel wall thickness 5.9. p analysis was <0.0001 which is remarkably significant and shows that in women with UAB compared to CG the number of vessels is 4 times greater, the diameter is 7.5 times greater, the vessel lumen 5.4 times greater and the vessel wall thickness is 9.8 times greater Table 2. There are no data in the literature that assess these findings in EMY in specimens from hysterectomies for any cause.
The literature review on abnormal vessels in the uterus only shows arteriovenous fistulas or uterine vascular malformations that have abnormal vessels throughout the thickness of the myometrium and extend to the serosa and Fallopian tubes, nothing is mentioned about alterations in vessels at the EMY [12-16].
According to the studies that show the frequency of known and unknown causes according to the PALM-COEIN classification, the unknown causes range between 45.9% (Hall [13]) and 12.4% (Ansari[8]). It is possible that this group includes UAB, which in our case series has a frequency of 7.5% (39/520). UVH is not independent of the findings in the endometrium already mentioned, since the arteries that feed the endometrium originate from the myometrium and correlate with the findings in the measurements of the vessels of Mintz [15] and ours in the UAB and should give rise to new studies with a comprehensive approach to explain the UAB more adequately.
Conclusion
For the first time, the possible cause of idiopathic UAB or of unknown cause is described according to the PALM-COEIN classification, which consists of the presence of abnormal vessels with an increase in the quantity, external diameter, wall thickness and diameter of the lumen that compared to CG and is between 4 to 9.8 times greater, this explains UAB due to the increase in blood flow.
Acknowledgments to case contributors:
Aguinaga Funes Francisco Alfonso MD, Bañuelos Jessica MD, Barla Muñoz Emma Elizabeth MD, Caballero Castaneda Iliana MD, Carreño Solía María Elena MD, García Wrooman José Manuel MD, Goroztizaga González Gerardo MD, León Gayosso Rosario MD, López Chávez Alejandra Gabriela MD, Martínez Bardales Carlos MD, Mancilla Bojorquez Drucila MD, Orizaba Chávez Bernardett MD, Ortega Ruíz Rosario MD, Peña Aguilar José María MD, Pérez Alcantara Griselda MD, Pérez Medrano Luis Ramón MD, Roa Quintanar David MD, Silva Palma Perla Angélica MD, Solís Loria Waldemar Alejandra MD, Torres Colín José MD, Valiente Banuet Guadalupe MD, Velasco Merlos Ana Alicia MD, Velázquez Fonseca Julián MD
References
- National Collaborating Centre for Women’s and Children’s Health. Heavy menstrual bleeding. (Ch. 3). (2007).
- Munro MG, Critchley HOD, Fraser IS (2018) The two FIGO systems for normal and abnormal uterine bleeding symptoms and classification of causes of abnormal uterine bleeding in the reproductive years: 2018 revisions. Int. J. Gynecol. Obstet. 143(3): 393–408.
- Royal College of Obstetricians and Gynecologists. National heavy menstrual bleeding audit final Report. 2014 (Ch. 1).
- https://www.rcog.org.uk/globalassets/documents/guidelines/research-audit/national_hmb_audit_final_report_july_2014.pdf (2014).
- Fraser IS, Langham S, Uhl-Hochgraeber K (2009) Health- related quality of life and economic burden of abnormal uterine bleeding. Expert Rev. Obstet. Gynecol. 4(2): 179–189.
- Shapley M, Jordan K, Croft PR (2004) An epidemiological survey of symptoms of menstrual loss in the community. Br. J. Gen. Pract. 54(502): 359–363.
- Jain V, Munro MG, Critchley HOD (2023) Contemporary evaluation of women and girls with abnormal uterine bleeding: FIGO Systems 1 and 2. Int J Gynecol Obstet. 162(Suppl 2): 29-42.
- Middelkoop MA, Don EE, Hehenkamp WJK, Polman NJ, Griffioen AW, et al. (2023) Angiogenesis in abnormal uterine bleeding: a narrative review. Hum Reprod Update. 29(4): 457- 485.
- Ansari A, Urooj U (2020) Study of causes behind abnormal uterine bleeding according to PALM- COEIN classification at a tertiary care hospital. J Pak Med Assoc. 70(1): 154-157.
- Blaustein A, Kurman RJ, Ellenson LH, Ronnett BM (2014) Patología del tracto genital femenino Blaustein. Venezuela; Ed AMOLCA; 7ª edición; Enfermedades benignas del endometrio, Capitulo. 7 pag 307-354.
- Mazur MT, Kurman R (2006) Diagnostico de biopsias y legrados endometriales. Buenos Aires Argentina: Ediciones Journal SA, Cap 5: 100-120.
- Huang E, Hornstein MD, Stewart EA, Crum PC, Evaluation of the cyclic endometrium and benign endometrial disorders Chap 16, pag 407-456 in Crum CP, Nucci MR, Lee KR. Diagnostic Gynecologic and Obstetric Pathology. Philadelphia USA: Elsevier Saunders, 2011; 2nd Ed.
- Goldblum JR, Lamps LW, McKenney JK (2017) Rosai and Ackerman’s Surgical Pathology. Philadelphia USA: Elsevier Saunders; 11th Ed.
- Hall EM, Ravelo AE, Aronoff SC, Del Vecchio MT (2024) Systematic review and meta-analysis of the etiology of heavy menstrual bleeding in 2,770 adolescent females. BMC Women’s Health. 24(1): 136.
- Ni P, Wu M, Guan H, Yuan Y, Zhang L, et al. (2022) Etiology distribution of abnormal uterine bleeding according to FIGO classification system: A combined study of ultrasound and histopathology. J Obstet Gynecol Res. 48(7): 1913-1920.
- Mints M, Hultenby K, Zetterberg E, Blomgren B, Falconer C, et al. (2007) Wall Discontinuities and increased expression of vascular endothelial growth factor-A and vascular endothelialgrowth factor receptors 1 and 2 in endometrial blood vessels of women with menorrhagia. Fertility and Sterility. 88(3): 691-7.
- Hapangama DK, Bulmer JN (2016) Pathophysiology of heavy menstrual bleeding. Womens Health (Lond). 12(1): 3-13.