Piotr Godek
Sutherland Medical Center, Warsaw, 04-036 Poland, ORCID ID: 0000-0001-7809-1289
*Corresponding Author: Piotr Godek, Sutherland Medical Center, Warsaw, 04-036 Poland, ORCID ID: 0000-0001-7809-1289
Abstract
Background: Lumbar foraminal stenosis (LFS) is a common form of spinal spondylosis, especially in the lower segments of the spine. It is usually a consequence of degenerative disc disease (DDD) leading to intervertebral instability and secondary hypertrophy of the intervertebral joints (facet joints) and ligamentous elements, creating a significant obstacle in the path of nerve roots leaving the spinal canal. The consequence of this entity is a mixed form of axial and radicular pain in patients with LFS. The prevalence of LFS has been reported to be 8–11 %. While the diagnosis of LFS based on imaging studies is not difficult, its conservative treatment causes considerable difficulties, not only because of the mechanical obstacle but most of all the perineural adhesions which are the cause of disturbed neurodynamic of the nerve roots and frequent pain chronification. The hyaluronic acid (HA) can be a new option for LFS symptomatic treatment as an interposing agent preventing perineural friction and the formation of adhesions around nerve roots.
Results: A 66-year-old, male patient, without a history of spine surgery, a blue-collar worker with pain in the lumbar region radiating to the left buttock and hip in the course of LFS, was referred by a physiotherapist due to ineffective manual therapy. The pain intensified after exertion, especially after working on a forklift, without any traumatic background. In a physical examination, positive Kemp's sign significantly reduced Straight Leg Raise (SLR) and positive Slump test on the left, no neurological deficiency symptoms. Radiography of the hip joints - no pathologies were found. In MRI, multi-level discopathy, foraminal stenosis of L4/L5 and L5/S1 segments predominately on the left. Due to severe pain, an ultrasound-guided steroid was administered around facet joints at the L5/S1 and L4/L5 levels. A month later, the patient came for a check-up reporting only a few days' improvements after administration of the steroid. In the medical survey, his condition did not differ from before the injection. Under ultrasound guidance, HA was administered epidurally (interlaminar approach) into the lateral recess at the L5/S1 level on the left side, and the patient was instructed how to perform neural mobilization exercises in the unloaded position. Follow-up after 4, 8 and 12 weeks confirmed sustained improvement in the Numeric Rating Scale, NRS (0-10), Oswestry Disability Index, ODI (0-50), Rolland-Morris Questionnaire, RM (0-24), and pain-free elevation angle in SLR test. There were no signs of intolerance to the HA and no administration complications.
Conclusion: Epidural hyaluronic acid injection combined with an exercise program can be an interesting way to improve nerve root neurodynamics in LFS and an alternative to steroid administration.
Keywords: Hyaluronic Acid; Spondylosis; Injections, Epidural.
Introduction
Lumbar foraminal stenosis (LFS) is a quite common form of spinal spondylosis, especially in the lower segments of the spine and it is the phenomenon of limited space of the lateral part of the spinal canal leading to compression of the root and dorsal root ganglion. In 1976, a definition and classification of LFS were proposed as an extension of the concept of spinal canal stenosis [1].
Anatomically, LFS describes the diameter of the intervertebral foramen and the volume of the lateral part of the spinal canal called the lateral recess, where several sensitive zones are distinguished. The anatomical boundaries for foramen are composed of multiple anatomical components: the adjacent vertebra pedicles, the posterior margins of adjacent vertebral bodies, the intervertebral disc (IVD), the ligamentum flavum, and superior and inferior articular facets as the posterior boundaries. The lateral canal is segmented into the lateral recess, vertical interpedicular (foraminal), and extraforaminal zone. The foraminal area varies from 40 to 160 mm 2 but not all space is available for the root because trans- or intra-foraminal ligaments are present in the inferior foraminal aspect. Thus, the exiting nerve root or dorsal root ganglion (DRG) surrounded by fat and radicular vessels is often located in the superior and anterior region of the foramen or in the subpedicular notch, normally occupying approximately 30 % of the available foraminal area. The most sensitive zone is where the arc of bending root in the subpedicular notch adheres to the cortical bone of the pedicle and where the root rubbing against its bone boundary is exposed to ischemia. In the course of degenerative spondylosis, the intervertebral foramen and the lateral recess decrease not only due to the hypertrophy of the facet joints, the ligamentum flavum, and the base of the arch but also due to the instability causing articular subluxation so the irregular course of the intervertebral foramen, changes its shape from vertical to oblique or even horizontal [2].
The prevalence of lumbar foraminal stenosis has been reported to be 8–11 %, specifically L5 nerve root disorders due to L5/S1 foraminal stenosis have been reported to account for 75 % of all cases of foraminal stenoses [3].
The LFS is often difficult to diagnose, contributing to an unfavorable prognosis after routine surgical treatment of lumbar spinal canal stenosis. In their review of failed back surgery syndrome, Burton et al. considered foraminal stenosis to be the cause of pain in nearly 60% of patients with persistent postoperative symptoms [4]. Although there are differences in clinical features of LFS, the clinical picture includes mixed axial and radial pain of the sciatica type, occurring not only during exercise but also at rest, and much more often than in the central form of spinal stenosis (76 vs. 35%) as confirmed by an intraoperative study by Yamada et al [5].
Conventional radiography is highly insufficient to assess the morphology and degree of lateral recess stenosis, therefore MRI is the best imaging modality in combination with CT, as the bone proliferative changes, soft tissue hypertrophy, and an accurate assessment of the degree of intervertebral disc degeneration are possible. The vacuum phenomenon and late stage of IVD pathology are encountered in the L5/S1 segment in 95.2% of the LSFS patients [6].
Due to the prolonged adherence of the root nerve to the bone boundaries and overgrown ligamentous elements, without the possibility of its natural movement in the physiological range, a few dangerous processes can occur that threaten the neurotrophy. Direct pressure exerted on the vasa nervorum with a blood supply deficit slows down the cytoplasmic transport and consequently promotes the neurodegenerative processes. On the other hand, the swelling and increased intra-nerve pressure due to the venous and lymphatic stasis of the root leads to further root ischemia because of increased vascular resistance. An additional unfavourable consequence of prolonged adherence is perineural adhesions, which arise especially abundantly in the inflammatory environment and can be visible in epiduroscopy images. All those mechanisms disturb the neurodynamics of the root and its dural sheet, leading to the formation of pernicious vicious circle: pressure => ischemia => swelling => inflammation => adhesion formation => ischemia => pressure [7].
The cause-oriented treatment of LFS is the removal of the mechanical obstacle, the release of adhesions, and the prevention of secondary stenosis using implants widening not only the diameter of the intervertebral foramen but also the volume of the lateral recesses (resections of the facet joints and ligaments).
In the symptomatic treatment of LFS, the attempt of mechanical widening of the lateral recess by traction procedures and manual therapy or local and systemic anti-inflammatory treatments (epidural and periradicular steroid injections) are commonly used. The conservative treatment faces however significant obstacles due to the rapid pain chronification because DRG located in the vicinity is prone to secreting from glial cells many substances that promote neuropathic pain like substance P and proinflammatory cytokines [8].
The concept of hyaluronic acid (HA) administration in the epidural space was initially introduced in animal studies. Its purpose was to interpose a dural sac with a slip layer to prevent adhesions and enable it to slide properly during normal movement.
In the case report presented here, the rationale for HA epidural administration assumes its contribution for regaining of normal nerve root neurodynamic, spontaneous resolution of radicular edema subjected to neural mobilization processes with the recovery of proper blood supply which will relieve the neuropathic pain in the long-term perspective.
Case report
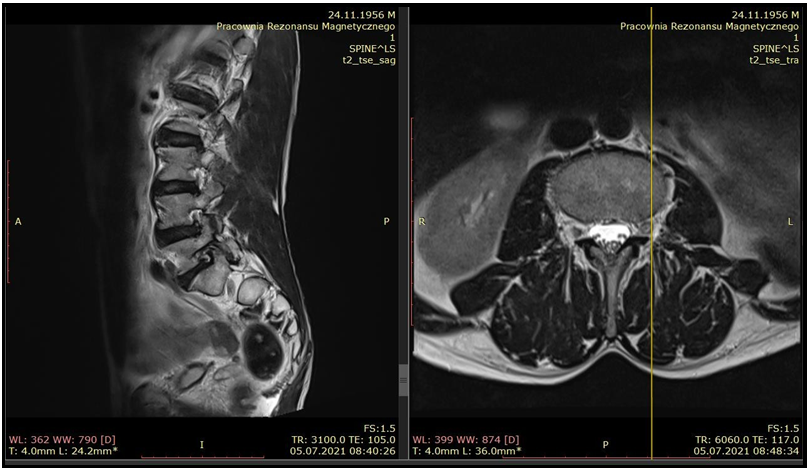
A 66-year-old, male patient, with a normal BMI, without a history of spine surgery, a blue-collar worker with pain in the lumbar region and its radiation to the left buttock and hip in the course of LFS, was referred by a physiotherapist due to ineffective manual therapy. The pain intensifies after exertion, especially after working on a forklift, without any traumatic background. In a physical examination, positive Kemp's sign on the left, significantly reduced SLR on the left side (45 degrees), on the right side 70 degrees, and positive Slump test. No neurological deficiency symptoms. Radiography of the hip joints - no pathologies. In MRI, multi-level discopathy, foraminal stenosis of L4/L5 and L5/S1 segments predominately on the left [Figure 1].
Figure 1: Lumbar spine MRI sagittal and transverse scan - foraminal stenosis of L4/L5 and L5/S1 segments.
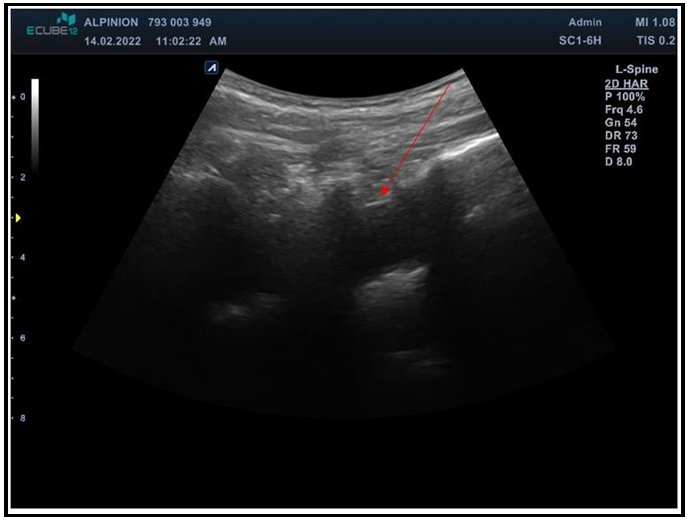
Due to severe pain, ultrasound-guided injection of steroid (Dexaven, 4 mg) was administered around the facet joints at L5/S1 and L4/L5 levels. A month later, the patient came for a check-up visit reporting only a few days' improvements, and in the medical survey, his condition did not differ from that before the injection. The patient was thoroughly informed about the possible reasons for the ineffectiveness of the current treatment and the options of further treatment were thoroughly explained to him, including the unconventional solution of HA ultrasound-guided epidurally in the area of the entrapped root as preparation for neural mobilization exercises. The patient accepted this option, reluctantly thinking about surgical treatment and continuing to take high doses of analgesics. Under ultrasound guidance, a single dose of HA (Synovial HL, IBSA) was administered epidurally (interlaminar approach, BD Spinal needle, 20G x 3,5’’) into the lateral recess at the L5/S1 level on the left side after the initial injection of 10 ml saline according to the loss of resistance method [Figure 2,3].
Figure 2: Ultrasound image of L5/S1 interlaminar acoustic window for epidural injection technique. Parasagittal long axis scan.
Figure 3: Ultrasound-guided L5/S1 interlaminar epidural injection. In-plane technique, starting point from caudal direction.
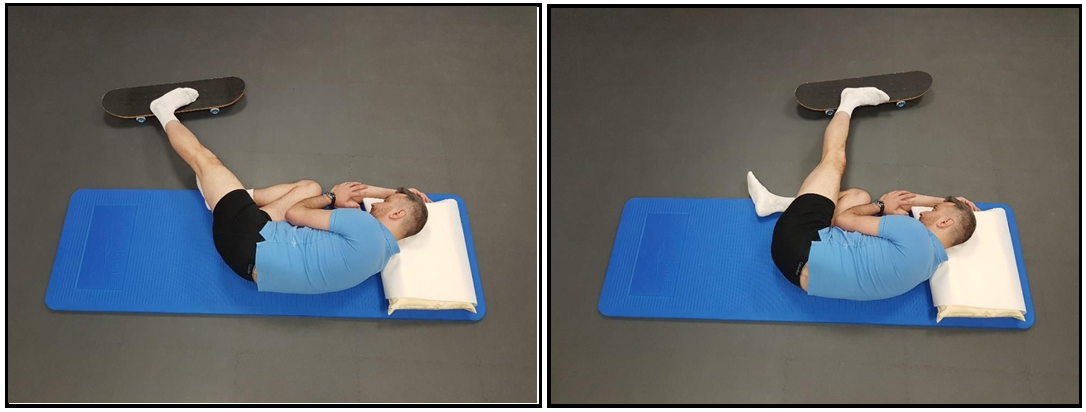
The injection was performed very slowly and gradually with constant monitoring of foot active movement for which the patient was encouraged. After 30 min observation, the patient was instructed how to exercise neural mobilization of the ischial nerve in the unloaded position of the spine (lateral decubitus with lumbar flexion) using a skateboard daily [Figure 4].
Figure 4: Neural mobilisation of the L5 root in autotherapy.
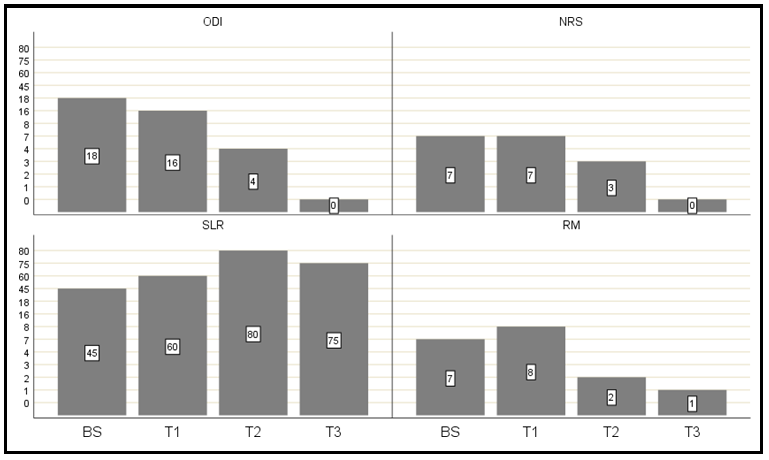
The patient was allowed to take intraoral anti-inflammatory agents in case of need in standard doses. No MRI imaging was scheduled in follow-up. The primary outcomes were: Numeric Rating Scale, NRS (0-10), Oswestry Disability Index, ODI (0-50), Rolland-Morris Questionnaire, RM (0-24), and pain-free elevation angle in the Straight Leg Raise, SLR test. The assessment was performed 4 (T1), 8 (T2), and 12 (T3) weeks after intervention. The evolution of outcomes values compared to baseline (BS) presents. [Figure 5].
Figure 5: Evolution of measured outcomes during follow-up.
There were no signs of intolerance to the HA and no administration complications, and finally, the patient got rid of the medications and returned to normal professional duties.
Discussion
Injections of HA are a common method of symptomatic treatment of osteoarthritis (OA), and although there is serious controversy among experts as to their true effectiveness, as they do not change the natural history of OA, many publications confirm that they at least improve the quality of life of patients with mild and moderate forms of OA [9]. In the field of plastic surgery, HA has long been used as a prophylactic agent for postoperative adhesions. This assumption was also made by Wang et al. when testing cross-linked hyaluronic acid gel applied epidural in an in vivo animal experimental study in rabbits. In their studies, they investigated cross-linked hyaluronic acid gel in the regulation of scar gene expression, the accumulation of fibroblasts in scar tissue, and the prevention of epidural adhesion after laminectomy. The effect of the cross-linked hyaluronic acid gel on the secretion of inflammatory factors was observed in vitro. In addition, to ensure the accuracy and reliability of the in vivo gene expression results, they used a cell model to detect the target genes in vitro. Histomorphometry results demonstrated that the number of fibroblasts in the experimental group was significantly lower than that in the control group 2 weeks postoperatively. Micro-CT scans showed that the cross-linked hyaluronic acid gel could reduce adhesion in the epidural space after laminectomy. Additionally, the cross-linked hyaluronic acid gel could inhibit IL-6 secretion [10].
Isik et al. reached similar conclusions in animal experiments using cross-linked high-molecular-weight hyaluronic acid applicated to rats that underwent laminectomy and discectomy. The experiment showed significantly lower fibroblast cell density and tissue hydroxyproline concentrations versus the control group. There was statistically significant lower dural adhesion and foreign-body reaction between the control and HA gel groups. Granulation tissue and epidural fibrosis were significantly lower in the HA and HA gel groups compared with the sham group [11].
Liu et al determined by the somatosensory evoked potentials that application of medical self-crosslinking sodium hyaluronate gel is effective on epidural scar adhesion after laminectomy in rabbits [12]. The HA is not just a lubricant. It also shows immunosuppressive and cytoprotective effects (increases ATP stores, increases DNA integrity, scavenges free radicals), anti-inflammatory effect by reducing the expression of genes for pro-inflammatory cytokines (IL-G), reducing the production of prostaglandins and metalloproteinases through the CD44 receptor, stimulates the endogenous production of HA, it also has an analgesic effect by lowering the input from free nerve endings by inhibiting substance P in nociceptors and reducing hyperalgesia messengers: PGE2 and bradykinin, while lowering the threshold of excitability of opioid receptors in the descending opioid system [13].
To the best knowledge of the author, there is no existing report of epidural HA administration in human subjects. The rationale for the presented procedure was to create an interposition slip layer for the L5 root sheaths in a tight lateral recess, thanks to which it would be possible to regain its natural mobility, which, according to the available literature, provides it with the correct trophic and inflammatory edema resolution [14].
For this purpose, after the initial administration of saline to obtain a niche for HA volume, very gentle mobilization of the L5 root was introduced through the sciatic nerve tract, within a pain-free range of motion. The unloaded position of the spine (lateral decubitus in the flexion position), which naturally favored the widening of the intervertebral foramina, provided optimal conditions for neural mobilization. The application of Sinovial HL 3.2 % (IBSA) with a hybrid composition of double weight molecules was selected for the therapy for several reasons: 1) highly purified product obtained in the fermentation process - a product that does not cause allergic reactions to animal products, 2) a small volume of injectate - 2 ml, 3) product registration allows for its extra-articular administration (e.g. around the tendons), 4) the double size of particles (High molecule weight, HMW + Low molecule weight, LMW) provides, with very good rheological properties thanks to HMW, while at the same time the endogenous HA production can be launched by LMW fraction by stimulation of fibroblasts available in the spinal canal, 5) no cytotoxic effect confirmed by trials reporting very good tolerance of the Synovial HL administered together with PRP [15,16,17,18].
A three-month follow-up with a sustained analgesic effect and an improvement in function observed in the SLR test seems to confirm the rationale for HA implementation as a factor contributing to neurodynamics improvement. It can be an incentive for further research that may open new opportunities in the field of conservative treatment of nerve root impingement syndromes due to perineural adhesions in the course of perineural inflammation. The further stage of research on the use of HA could cover a pilot study on a larger group of patients or a blinded randomized prospective study with a control group.
Conclusion
Epidural hyaluronic acid injection combined with an exercise program can be an interesting way to improve nerve root neurodynamics in LFS and an alternative to steroid administration.
Disclosures: The authors declare no financial disclosures and conflict of interest.
References
- Arnoldi CC, Brodsky AE, Cauchoix J, Crock HV, Dommisse GF, et al. (1976) Lumbar spinal stenosis and nerve root entrapment syndromes. Definition and classification. Clin Orthop Relat Res. 115: 4–5.
- Orita S, Inage K, Eguchi Y, Kubota G, Aoki Y, et al. (2016) Lumbar foraminal stenosis, the hidden stenosis including at L5/S1. Eur J Orthop Surg Traumatol. 26(7): 685-693.
- Jenis LG, An HS (2000) Spine update: lumbar foraminal stenosis. Spine. 25(3): 389–394.
- Burton CV, Kirkaldy-Willis WH, Yong-Hing K, Heithoff KB (1981) Causes of failure of surgery on the lumbar spine. Clin Orthop Relat Res. (157): 191-199.
- Yamada K, Aota Y, Higashi T, Ishida K, Nimura T, et al. (2014) Lumbar foraminal stenosis causes leg pain at rest. Eur Spine J. 23(3): 504-507.
- Ohba T, Ebata S, Fujita K, Sato H, Devin CJ, et al. (2015) Characterization of symptomatic lumbar foraminal stenosis by conventional imaging. Eur Spine J. 24(10): 2269-2275.
- Choi YK (2019) Lumbar foraminal neuropathy: an update on non- surgical management. Korean J Pain. 32(3): 147-159.
- Esposito MF, Malayil R, Hanes M, Deer T (2019) Unique Characteristics of the Dorsal Root Ganglion as a Target for Neuromodulation. Pain Med. 20(Suppl 1): S23-S30.
- Maheu E, Bannuru RR, Herrero-Beaumont G, Allali F, Bard H, et al. (2019) Why we should definitely include intra-articular hyaluronic acid as a therapeutic option in the management of knee osteoarthritis: Results of an extensive critical literature review. Semin Arthritis Rheum. 48(4): 563-572.
- Wang K, Li XL, Liu J, Sun X, Yang H, et al. (2020) Using cross- linked hyaluronic acid gel to prevent postoperative lumbar epidural space adhesion: in vitro and in vivo studies. Eur Spine J. 29(1): 129-140.
- Isık S, Taşkapılıoğlu MÖ, Atalay FO, Dogan S (2015) Effects of cross-linked high-molecular-weight hyaluronic acid on epidural fibrosis: experimental study. J Neurosurg Spine. 22(1): 94-100.
- Liu H, Li HF, Wang JY (2014) Prevention effect of medical self- crosslinking sodium hyaluronate gel on epidural scar adhesion after laminectomy. Asian Pac J Trop Med. 7(6): 501-504.
- Gupta RC, Lall R, Srivastava A, Sinha A (2019) Hyaluronic Acid: Molecular Mechanisms and Therapeutic Trajectory. Front Vet Sci. 6: 192.
- Ellis R, Carta G, Andrade RJ, Coppieters MW (2021) Neurodynamics: is tension contentious?. J Man Manip Ther. 1-10.
- Scaturro D, Vitagliani F, Terrana P, Cuntrera D, Falco V, et al. (2021) Intra-Articular Hybrid Hyaluronic Acid Injection Treatment in Overweight Patients with Knee Osteoarthritis: A Single-Center, Open-Label, Prospective Study. Applied Sciences. 11(18): 8711.
- Migliore A, Blicharski T, Plebanski R, Zegota Z, Gyula G, et al. (2021) Knee Osteoarthritis Pain Management with an Innovative High and Low Molecular Weight Hyaluronic Acid Formulation (HA-HL): A Randomized Clinical Trial. Rheumatol Ther. 8(4): 1617-1636.
- Papalia R, Zampogna B, Russo F, Torre G, De Salvatore S, et al. (2019) The combined use of platelet rich plasma and hyaluronic acid: prospective results for the treatment of knee osteoarthritis. J Biol Regul Homeost Agents. 33(2 Suppl. 1): 21-28.
- Conforti M (2020) Combination of laser needling and hyaluronic acid infiltration treatments for rotator cuff calcific tendinopathies. Gazzetta Medica Italiana-Archivio per le Scienze Mediche. 179(12): 665-74.