Jimena Alejandra Anchava1*, Karina Alejandra Melian2, Marina Andrea Toscano3
1Universidad de Buenos Aires, Facultad de Odontología, Cátedra de Odontología Integral Niños, Buenos Aires, Argentina. ORCID: https://orcid.org/0009-0002-7486-1746
2Universidad de Buenos Aires, Facultad de Odontología, Cátedra de Odontología Integral Niños, Buenos Aires, Argentina. ORCID: https://orcid.org/0009-0006-3493-8533
3Universidad de Buenos Aires, Facultad de Odontología, Cátedra de Odontología Integral Niños, Buenos Aires, Argentina. ORCID: https://orcid.org/0009-0005-7093-5041
*Corresponding Author: Jimena Alejandra Anchava, Universidad de Buenos Aires, Facultad de Odontología, Cátedra de Odontología Integral Niños, Buenos Aires, Argentina. ORCID: https://orcid.org/0009-0002-7486-1746
Abstract
The estimated global prevalence of traumatic dental injuries (TDI) in the permanent dentition is 15.2%. When a tooth is able to absorb the impact force, a crown fracture is highly likely to occur. These fractures are among the most common reasons for emergency consultations in pediatric dentistry, with maxillary central incisors being the most frequently affected. Crown fractures may be limited to enamel, involve dentin, or extend to the pulp tissue, which influences the prognosis and determines the therapeutic approach. The restoration of coronal integrity must respect the shape, color, and surface texture of the affected teeth. Enamel-dentin fractures without pulp exposure are usually managed with conservative adhesive techniques, while the approach becomes more complex when pulp tissue is involved. In cases where pulp vitality cannot be preserved, endodontic treatment is indicated, followed by the placement of a radicular post and the fabrication of an artificial core build-up for subsequent prosthetic rehabilitation. Although treatment guidelines and protocols are available, each case presents specific characteristics that require an individualized, evidence-based approach. The aim of this paper is to present the clinical management of various types of crown fractures following TDI, emphasizing the importance of personalized treatment and long-term follow-up.
Keywords: Permanent Dentition; Tooth Injuries; Tooth Fractures; Composite Resins; Computer-Aided Design
Introduction
Traumatic dental injuries (TDI) have increased in frequency in recent years, with a global prevalence of 15.2% in the permanent dentition. These injuries are among the most frequent reasons for consultation in pediatric dentistry and can cause significant psychological, economic, functional, and aesthetic repercussions, affecting individual, family, and social patients’ quality of life [1, 2].
If the tooth absorbs the impact force, it is highly likely that a crown fracture will occur. Crown fractures are among the most common traumatic injuries in young permanent dentition, with a prevalence ranging from 26% to 76% between the ages of 8 and 10, most frequently affecting the maxillary central incisors. These fractures may be limited to the enamel, involve the dentin, or extend to the pulp tissue, influencing the prognosis and guiding the therapeutic approach [1, 3, 4].
The clinical management of these fractures depends on multiple factors, such as the extent of the damage, the stage of root development, the time elapsed since the trauma, the presence of symptoms, and the possibility of preserving the tooth fragment. Enamel-dentin fractures without pulp exposure are usually treated with conservative adhesive techniques. In contrast, when pulp exposure is present, vital pulp therapies such as direct pulp capping or pulpotomy are required, especially in immature teeth. When pulp vitality cannot be maintained, endodontic treatment is indicated, followed by the placement of a radicular post and the fabrication of a core build-up for subsequent prosthetic rehabilitation [5–10].
Although there are treatment guidelines and protocols, each situation requires an individualized approach guided by the available scientific evidence [6, 11]. Accurate clinical and radiographic evaluation, along with a precise diagnosis, is essential for selecting the most appropriate intervention and promoting tissue healing. An interdisciplinary approach, along with long-term follow-up, is essential to ensure the functional, structural, and aesthetic health of the traumatized tooth [1, 3, 12].
This report presents the clinical management of crown fractures of varying severity: an enamel-limited fracture, an enamel-dentin fracture without pulp involvement, and a complicated fracture with pulp exposure, highlighting the importance of individualized treatment and long-term follow-up.
Case Report
A 10-year-old female patient presented for consultation after suffering a traumatic injury at school during play volleyball, caused by a blow to the chin against the floor, which had occurred seven days prior to her visit to Cátedra de Odontología Integral Niños de la Facultad de Odontología de la Universidad de Buenos Aires.
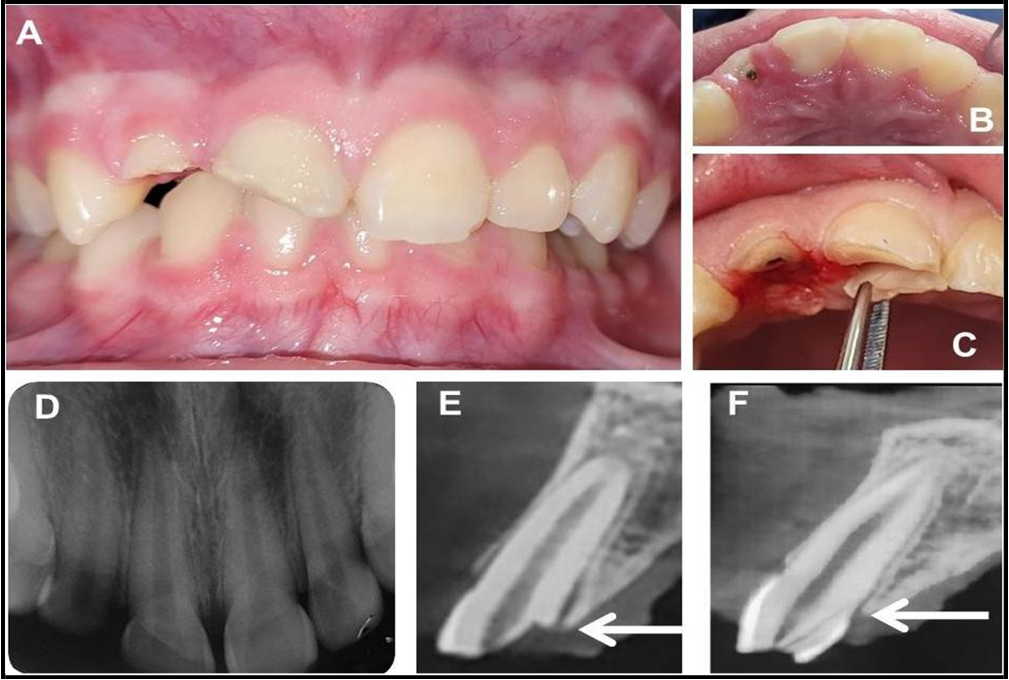
Clinical examination revealed a complicated crown fracture involving the cervical third of tooth 1.2, an uncomplicated crown fracture of tooth 1.1, and an enamel fracture of tooth 2.1 (Figure 1A-B-C). Radiographically, complete root formation of the affected incisors and their antagonists was observed (Figure 1D). A cone-beam computed tomography (CBCT) scan with 1 mm slices was requested, which confirmed the diagnosis (Figure 1E-F).
Figure 1: (A) Frontal photograph showing the crown fractures. (B–C) Occlusal photographs showing the fracture lines in teeth 1.1 and 1.2. (D) Initial periapical radiograph. (E–F) Cone-beam computed tomography (CBCT), sagittal slices, showing crown fractures in teeth 1.2 and 1.1.
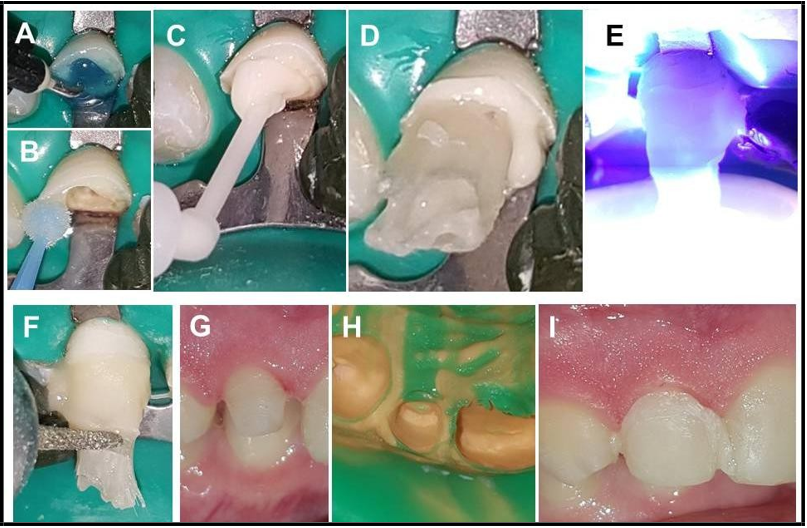
After obtaining informed consent and the patient’s assent, the emergency situation was addressed. Tooth 1.2 underwent mechanized endodontic treatment, with obturation using the lateral condensation technique with gutta-percha cones and ADSEAL® endodontic sealer (Meta Biomed Co. Ltd., South Korea). In tooth 1.1, a pulp-dentin protection was performed using light-cured glass ionomer Fuji II LC® (GC Corporation, Japan) after fragment removal. In tooth 2.1, the enamel edge was polished since the lesion was limited to enamel. At the end of the session, chlorhexidine gluconate 0.12% mouth rinses, a soft diet, and temporary suspension of sports activities were indicated (Figure 2 A-B).
Figure 2: (A–B) Frontal and occlusal views of the pulp-dentin protection in 1.1 and post-endodontic temporay restauration in 1.2 with light-cured glass ionomer. (C) Heavy-body silicone matrix. (D-E) Diagnostic wax-up.
Seven days later, teeth 1.1 and 2.1 were definitively restored using selective enamel etching with 37% phosphoric acid (Ultra-Etch®, Ultradent Products Inc., USA), application of a universal adhesive system (One Coat 7®, Coltène/Whaledent AG, Switzerland), and stratification with dentin (A2/B2) and enamel (A3/D3) composite resins (Brilliant NG®, Coltène/Whaledent AG, Switzerland), following a diagnostic wax-up and silicone matrix fabrication (Figure 2C-D-E and Figure 3).
Figure 3: Sequence of composite resin restorations in 1.1 and 2.1. (A) Shade selection. (B) Flat enamel. (C) Selective enamel etching. (D) Application of adhesive system. (E) Stratification with composite resins. (F) Final clinical photograph.
For tooth 1.2, a radicular post was placed using long, continuous, unidirectional quartz fibers embedded in an unpolymerized resin matrix (Quartz Splint™ Unidirectional, RTD Dental, France). The canal was partially deobturated (8 mm) using a Gates Glidden bur, maintaining a 1:1 crown-root ratio. The canal was then irrigated with saline and dried with paper points. Glycerin was used as a separating agent. The fibers were inserted and laterally compacted using an endodontic spreader. After placement, the post was infiltrated with highly filled flowable resin (ENA® Hri®, Micerium S.p.A., Italy), light-cured for 5 seconds to allow removal of the customized post, and then fully cured outside the canal (Figure 4).
Figure 4: (A - B) Initial clinical and radiographic photographs. (C) Partial removal of the root canal filling material. (D) Long, continuous, unidirectional quartz fibers impregnated in a non-polymerized resin matrix. (E) Lateral condensation of fibers inside the canal. (F - G) Infiltration with highly filled flowable resin prior to initial light curing. (H) Individualized quartz fiber post.
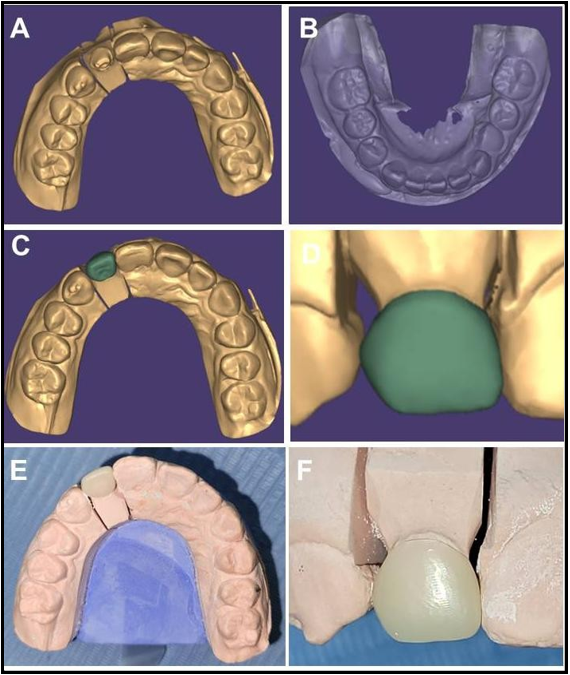
The remaining tooth structure and the post were treated to allow bonding with resin cement (ParaCore® Slow, Coltène/Whaledent AG, Switzerland), and the excess fibers were trimmed. Tooth preparation and impression were carried out in a single stage using light-body and heavy-body addition silicone (President®, President Dental GmbH, Germany). A provisional crown was fabricated with bis-acrylic resin (Structur 2®, VOCO GmbH, Germany) using a silicone matrix derived from the diagnostic wax-up (Figure 5).
Figure 5: (A-B-C-D) Bonding of the post with resin cement. (E) Fotopolimerization (F) Trimming of the excess fibers. (G-H) Preparation and impression with light-body and heavy-body addition silicone. (I) Provisional crown with bisacrylic resin.
The models were digitally scanned, and the final crown was designed and fabricated from a reinforced composite block (Brilliant Crios®, Coltène/Whaledent AG, Switzerland) using subtractive CAD/CAM technology. It was cemented with ParaCore® Slow (Figure 6).
Figure 6: (A-B) Digitization of the models. (C-D-E-F) Design and fabrication of the definitive crown from a reinforced composite block using subtractive technique with CAD/CAM technology.
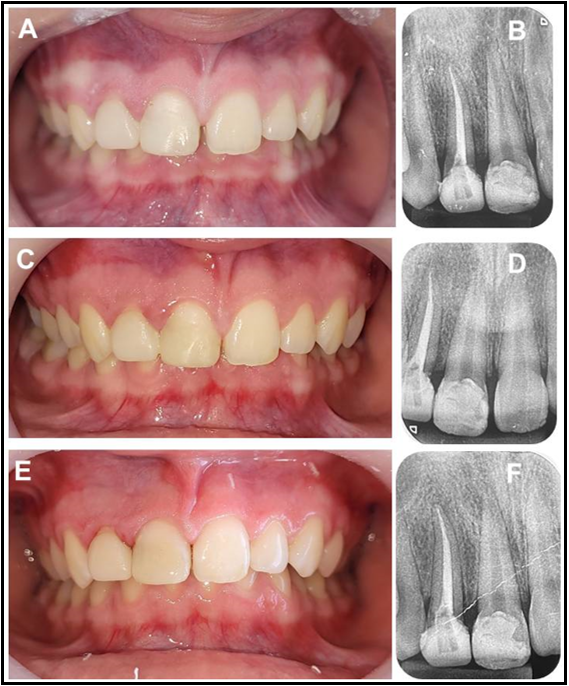
A customized mouthguard was fabricated, and clinical and radiographic follow-ups were scheduled at 1 month (Figure 7), 6 months, 1 year, and 2 years after comprehensive discharge (Figure 8). The patient exhibited good masticatory function, with no signs or symptoms of pulpal or periapical pathology, and satisfactory esthetics. The restorations remained in good condition, with no evidence of fractures, leakage, or marginal gap.
Figure 7: (A–B) Immediate clinical and radiographic follow-up. (C-D) One-month clinical follow-up and fitting of the custom mouthguard.
Figure 8: Clinical and radiographic follow-ups: (A-B) at 6 months, (C-D) at 1 year, and (E-F) at 2 years after treatment and complete rehabilitation.
Discussion
The diagnosis and treatment of TDI represent a significant clinical challenge, especially in pediatric patients [6, 13, 14]. This clinical case illustrates the diagnostic and therapeutic complexity of TDIs in the permanent dentition and highlights the importance of an interdisciplinary, individualized, and evidence-based approach.
The coexistence of three types of crown fractures of varying severity—enamel, enamel-dentin without pulp exposure,and complicated crown fracture—in a single patient posed a clinical challenge that required a differentiated treatment plan for each affected tooth, ranging from conservative procedures to complex rehabilitations involving radicular posts and CAD/CAM techniques. Several studies agree that the maxillary central incisors are the most frequently affected teeth by trauma in school-aged children, consistent with the findings in this case. The uncomplicated fractures in teeth 1.1 and 2.1 were treated with conservative adhesive techniques, achieving satisfactory long-term clinical and esthetic outcomes. The use of light-cured glass ionomer for pulp-dentin protection in the emergency session, followed by restoration with advanced composite resins, allowed excellent biological, functional, and esthetic integration. These procedures align with current recommendations from the International Association of Dental Traumatology (IADT) [6, 7, 10, 12, 14].
For the maxillary right lateral incisor, CBCT was essential to determine the exact extent of the fracture. Diagnostic difficulties are common, and clinicians’ ability to accurately identify specific injuries is crucial for optimal treatment planning. In this context, advances in 3D imaging technologies have improved both diagnostic accuracy and therapeutic planning. More accurate diagnoses significantly enhance clinical judgment and treatment outcomes [15, 16]. CBCT is especially useful in cases involving root fractures, crown-root fractures, and lateral luxations [6]. In this case, where crown-root fractures were suspected in teeth 1.2 and 1.1, the imaging was critical for establishing the treatment plan.
The decision to use a quartz fiber post was based on the limited amount of remaining tooth structure needed to restore the crown. These long, continuous, unidirectional fibers, embedded in an unpolymerized resin matrix, allow passive adaptation inside the root canal. Unlike prefabricated posts that require additional drilling, these fibers do not need post space preparation, preserving more of the remaining tooth structure. This approach follows the principles of minimally invasive dentistry, maximizing the preservation of dentin and optimizing the distribution of functional stress along the tooth's long axis. Moreover, the ability to customize the post enhances both bonding and biomechanical performance. This is particularly relevant in young teeth with weakened structures, as it helps preserve tooth integrity, reduce fracture risk, and improve stress distribution [8, 9, 17, 18].
Regarding the definitive rehabilitation of tooth 1.2, a subtractive CAD/CAM technique was chosen, using a hybrid submicron reinforced composite block (Brilliant Crios®) due to its mechanical properties, elastic compatibility with dentin, and its ability to absorb functional stresses. This option offers excellent marginal adaptation, high precision, favorable esthetics, and repairability, making it a recommended alternative for patients with complex restorative needs [19, 20]. The use of indirect adhesive materials allows for functional, esthetic, and durable restorations without further compromising the remaining tooth structure [21, 22].
The decision to fabricate a personalized mouthguard following comprehensive rehabilitation also aimed to prevent future injuries, especially considering the patient’s age and sport activity. This indication aligns with current TDI prevention guidelines, as mouthguards significantly reduce the risk of oral injuries in children engaged in contact sports or high-impact physical activities [6, 10, 23, 24].
Short-, medium-, and long-term clinical and radiographic follow-ups allowed for assessment of the treatment outcomes. After two years, the restorations remained stable, with excellent esthetic and functional results and no signs of pulpal or periapical pathology, confirming the effectiveness of the comprehensive approach.
Conclusions
The treatment of crown fractures in young permanent dentition must be tailored to the severity, extent, and root development of the affected tooth. Whenever possible, procedures should aim to preserve pulp vitality. Achieving this requires accurate clinical and adiographic diagnosis, as well as the selection of modern biomaterials and techniques that enable predictable restorations. Periodic follow- ups, along with the cooperation of the patient and their support network, are essential for therapeutic success and the prevention of future complications.
Funding
This study was self-funded by the authors.
Conflicts Of Interest
The authors declare that there are no conflicts of interest regarding the publication of this paper.
References
- Petti S, Glendor U, Andersson L (2018) World traumatic dental injury prevalence and incidence, a meta-analysis—One billion living people have had traumatic dental injuries. Dent Traumatol. 34(2): 71-86.
- Arhakis A, Athanasiadou E, Vlachou C (2017) Social and psychological aspects of dental trauma: behavior management of young patients who have suffered dental trauma. Open Dent J. 11(1): 41-47.
- Andreasen FM, Andreasen JO (2014) Fracturas de la corona. In: Andreasen JO, Andreasen FM, editors. Texto y atlas a color de las lesiones traumáticas a las estructuras dentales. 4th ed. Caracas: AMOLCA. 1(1): 280-313.
- Bertolino M, Melian K, Anchava J (2022) Prevalencia de traumatismos dentoalveolares en Cátedra Odontología Integral Niños (nro. 125). In: Libro de resúmenes de la LV Reunión Científica Anual; 2022 Oct 30-Nov 1; Buenos Aires, Argentina. Buenos Aires: Sociedad Argentina de Investigación Odontológica; 2022.
- Tasdemir T, Eymirli PS, Ileri T, Ozler CO, Turgut MD (2025) Management of crown fractures with different pulp treatments and re-attachment technique: case series. BMC Oral Health. 25(1): 489.
- Bourguignon C, Cohenca N, Lauridsen E, Flores MT, O'Connell AC, et al. (2020) International Association of Dental Traumatology guidelines for the management of traumatic dental injuries: 1. Fractures & luxations. Dent Traumatol. 36(4): 314-30.
- Eden E, Taviloğlu E (2016) Restoring crown fractures by direct composite layering using transparent strip crowns. Dent Traumatol. 32(2): 156-60.
- Trushkowsky RD (2014) Restoration of endodontically treated teeth: criteria and technique considerations. Quintessence Int. 45(7): 557-67.
- Sowmya M, Madhu Varma K, Kalyan Satish R, Manthena SRK, Sai Dinesh J, et al. (2020) Fiber-reinforced composites in endodontic practice: a review. Int J Dent Mater. 2(4): 122-34.
- Villalobos-Guevara LA, Wahn Sosa E, Turcios Bonilla JE (2025) Fracturas coronales complicadas: desde el manejo de emergencia hasta su rehabilitación. Informe de un caso. RCOE. 30(1): 643-9.
- Revista Odontopediatría Latinoamérica (2025) Manual de referencia para procedimientos en odontopediatría. 1st ed.
- Arbuckle L, Alani A, Calvert G (2023) Dental trauma: assessment and acute management of fractures. Prim Dent J. 12(4): 36-46.
- Zerman N, Cavalleri G (1993) Traumatic injuries to permanent incisors. Endod Dent Traumatol. 9(2): 61-4.
- Kuriakose MC, Nair R (2019) Esthetic management of complicated crown fracture in anterior teeth: a case report. Cons Dent Endod J. 4(2): 49-52.
- Cohenca N, Silberman A (2017) Contemporary imaging for the diagnosis and treatment of traumatic dental injuries: a review. Dent Traumatol. 33(5): 321-8.
- Van Gorp G, Maes A, Lambrechts M, Jacobs R, Declerck D (2023) Is use of CBCT without proper training justified in paediatric dental traumatology? An exploratory study. BMC Oral Health. 23(1): 270.
- Avcılar İH, Bakır Ş (2023) Use of fiber-containing materials in restorative dentistry. J Dent Sci Educ. 1(2): 49-54.
- Jain A, Shah NC, Kumar RSM, Dedania M, Purbey RK, et al. (2025) Intracanal reinforcement with direct composite buildup as an alternative to fiber posts: an in vitro analysis. J Conserv Dent Endod. 28(5): 431-8.
- Rexhepi I, Santilli M, D'Addazio G, Tafuri G, Manciocchi E, et al. (2023) Clinical applications and mechanical properties of CAD-CAM materials in restorative and prosthetic dentistry: a systematic review. J Funct Biomater. 14(8): 431.
- Furtado de Mendonca A, Shahmoradi M, Gouvêa CVD, De Souza GM, Ellakwa A (2019) Microstructural and mechanical characterization of CAD/CAM materials for monolithic dental restorations. J Prosthodont. 28(2): e587-94.
- Alshargawi WK, Tawhari FE, Aladwani AS, Hassanein ZA, Fageeh SN, et al. (2024) The effectiveness of direct versus indirect restoration techniques following canal therapy. Int J Community Med Public Health. 11(10)
- Krastl G, Krug R, Nolte D, Kielbassa AM (2022) Traumatized teeth: clinical practice guideline for the interim management of teeth with various poor prognosis scenarios in growing patients. Quintessence Int. 53(8): 722-31.
- Popovici C, Bordea IR, Inchingolo AD, Inchingolo F, Inchingolo AM, et al. (2025) Dental splints and sport performance: a review of the current literature. Dentistry J. 13(4): 170.
- Majewski M, Kostrzewska P, Ziółkowska S, Kijek N, Malinowski K (2022) Traumatic dental injuries - practical management guide. Pol Merkur Lekarski. 50(297): 216-8.