Sailaja Nandennagari1, Opeyemi Adeoye Owolabi2, Ukaamaka Maryann Ogbu2, Javairia Ayyub3, Preethi Annam1, Krupavaram Bethala4*
1Avalon University School of Medicine, Curaçao
2American University of Barbados school of Medicine, Barbados
3Caribbean Medical University School of Medicine, Curaçao
4KPJ Healthcare University College, Kuala Lumpur, Malaysia
*Corresponding Author: Krupavaram Bethala, KPJ Healthcare University College, Kuala Lumpur, Malaysia.
Abstract
Our case study focuses on distinguishing hyponatremia causes in males and females. Females are more prone than males for an array of reasons, including estrogen sensitization of antidiuretic hormone (ADH) receptors causing dilutional hyponatremia, increased expression of sodium chloride channels (NCC) in females, the fact that females drink more water than males, and females are more symptomatic than males. Thiazide-induced hyponatremia is one of the most unusual severe electrolyte disorders.
Keywords: Hyponatremia, estrogen, thiazides, etc.
Introduction
Thiazide is classified as a diuretic since it works on the distal tubules and helps to pass urine. Hydrochlorothiazide and chlorthalidone have been shown to be more useful in the African American population with hypertension. They are a family of medications that reabsorb 3 % to 5 % of the luminal sodium in the kidney's distal convoluted tubules. Three thiazide diuretics are routinely used: hydrochlorothiazide, chlorthalidone, and indapamide [1]. The most thiazide side effects include hypokalemia, metabolic alkalosis, hypercalcemia, hyperglycemia, hyperuricemia, hyperlipidemia, and hyponatremia, an electrolyte imbalance characterized by a blood sodium levels of less than 136 mEq/L. Hyponatremia is a high-risk condition that caninduce mild to moderate mental status changes such as disorientation.
Case Details
A 65-year-old female was admitted to the emergency room complaining of weakness, fatigue, dizziness, abdominal cramps, and confusion. The patient claims she is too fatigued even though she has not done much work at home for five days. For this reason, she consulted her primary care physician as she felt very uncomfortable. Her primary care physician checked her electrolytes, and she was found hyponatremic, 134 mEq/L, and she was referred to the emergency department. The patient was started on Chlorthalidone 25 mg/day for her recently diagnosed hypertension. Four days after the patient began taking her medication, she became too confused and fatigued later, followed by vomiting and abdominal cramps.
On arriving at the emergency room, the patient's vitals were stable, with a blood pressure of 100/60 mm of Hg. The patient's electrolytes were checked, and her values were average except for sodium of 133 mEq/L. Management included cessation of Chlorthalidone, regular diet with potassium replacement, and isotonic saline. Furthermore, the patient was replaced with loop diuretics (Furosemide) for her blood pressure. The patient was stable within three days, and she was discharged.
Discussion
Thiazide diuretics are considered the most cost-effective class of antihypertensive agents for reducing adverse hypertension outcomes, as demonstrated in the Systolic Hypertension in the Elderly (SHEP) trial and the more recent Antihypertensive and Lipid-lowering Treatment to Prevent Heart Attack Trial (ALLHAT) [2]. Thiazide diuretics are classified into two types: those that have the benzothiadiazinering structure, such as hydrochlorothiazide, and those that do not, such as chlorthalidone and indapamide [3]. Thiazide diuretics treat hypertension by inhibiting NaCl reabsorption in the distal convoluted tubule. They lower blood pressure and can help other antihypertensive medications work better, although concerns about metabolic alterations, including hyponatremia and hypokalemia, may restrict their usage [4]. When the Na/cl channel in the distal convoluted tubule is blocked, there is an increase in sodium and water retention in the lumen and a reduction in sodium in the DCT. Simultaneously, it enhances ion flow across the Na/Ca2+ channel, increasing calcium reabsorption into the interstitium in exchange for sodium return to the DCT. This results in sodium retention mediated by aldosterone and increased excretion of potassium and hydrogen ions in the urine [5].
Figure 1: Diuretics effects on kidney, adapted from smart.servier.com
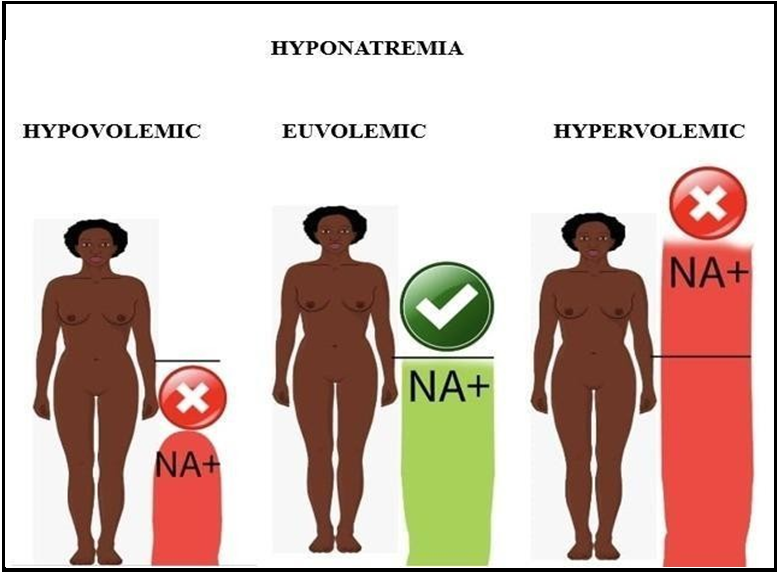
Criteria for Thiazide induced hyponatremia:
1. Euvolemia
2. Thiazide cessation leads improvement: 3 mEq/L in one day or 5 mEq/L in two days
3. Before Thiazide cessation: No significant improvements except with 3% NaCl, Urea or Vapton
4. No recurrence after cessation of Thiazide
Thiazide usage can cause hyponatremia, a dangerous and even deadly adverse effect in a small percentage of people. Age, feminine sex, low body mass, and genetic vulnerability are all risk factors. The reason is unknown; however, variables such as excessive fluid consumption, cation depletion, and a diminished capacity to excrete free water are considered involved. Depending on the population investigated, it can induce hyponatremia in up to 17 % of individuals. In the Systolic Hypertension Program, 4.1 % of thiazide diuretic-treated patients experienced hyponatremia, compared to 1.3 % in the control group [6,7].
In females,
Increased expression of sodium-chloride cotransporter channels (NCC) in females causes more significant sodium loss when thiazides inhibit NCC leading to concentrated urine due to water excess, compounded by mild volume depletion from thiazides. The average time for Thiazide-induced hyponatremia ranges from years, months, or even days, which may be due to the heterogeneity of the disease. Sometimes, the causes may be multifactorial, causing sodium depletion [8].
A more significant number of case reports state that hypertensive women may present with Thiazide-induced hyponatremia compared to men, whose reasons may be that women drank more water than men and were subjected to dilutional hyponatremia or more hypertensive women may be treated with diuretics than men or women may be more symptomatic than men for comparable sodium levels and may be diagnosed more often [9].
Estrogen stimulates Arginine Vasopressin and increases the sensitivity of ADH receptors retaining the fluids causing electrolyte dilution leading to dilutional hyponatremia and making females more susceptible compared to males [10].
Hyponatremia is a common electrolyte abnormality among medical inpatient individuals and affects up to one-third of elderly patients on thiazides. Hyponatremia occurs when serum sodium levels drop below 136 mEq/L, with symptoms including lethargy, headache, and nausea. As levels decrease, symptoms can progress to confusion, seizures, and irreversible brain damage below 120 mEq/L. For severe hyponatremia (Na below 125mM), thiazide diuretics are the leading cause in over a quarter of cases and cause drug-induced severe hyponatremia [11].
Thiazide-induced hyponatremia should be addressed by discontinuing the medications and infusing isotonic or hypertonic saline, depending on the severity of the hyponatremia. However, there is an imminent danger of overcorrection, and close monitoring is essential to prevent Osmotic demyelination, particularly in individuals with moderate to severe hyponatremia [12].
Figure 2: Types of hyponatremia, adapted from smart.servier.com
Differential Diagnoses
The production of excessive antidiuretic hormone (ADH) from the posterior pituitary gland is referred to as SIADH, which reduces the ability to eliminate diluted urine. At the same time, ingested fluid is retained, and extracellular fluid swells and becomes hypoosmolar. The key symptoms are hyponatremia, serum hyperosmolality, and little diluted urine. The most prevalent signs are weakness, stupor, headache, and weight gain, which may be followed by other symptoms that mirror psychiatric illnesses in most people. Another risk factor associated with the development of SIADH is smoking [13]
The deliberate ingestion of excessive water is connected with mental illnesses such as schizophrenia, bipolar disorder, and depression.
Hypothyroidism is a medical disorder caused by thyroid hormone insufficiency. An elevated antidiuretic hormone can cause a hypothyroidism-induced reduction in cardiac output.
Low salt consumption can also cause hyponatremia and a high mortality rate.
Conclusion
Asymptomatic patients will be benefited from Thiazide cessation and water restriction, while symptomatic patients may need either isotonic or 3 % hypertonic saline, which again depends on the severity of hyponatremia. Understanding pathophysiology, risk factors, and complications might help rationalize using this group of medicines.. Our case study highlights that the estrogen effect makes females more susceptible than males. This case study suggests that Thiazide use should not be generalized to prescribe for all recently diagnosed hypertensive patients and it also enhances case-based learning for medical students, resulting in better understanding and analysis. As most practitioners start the Thiazide group of drugs for blood pressure as a starting medication, understanding potential complications, especially in females, is vital.
Authors Contributions: All the authors contributed equally to the case report
Patient consent to publish: The patient’s verbal and written permission was obtained
Conflict of Interest to Publish: The authors declare no conflict of interest in this work
Peer Review: External peer review done
Funding: No funding received
Abbreviations
ADH: Antidiuretic hormone
ALLHAT: Antihypertensive and Lipid-lowering Treatment to Prevent Heart Attack Trial
DCT: Distal convoluted tubule Na: Sodium
Na/Ca2+: Sodium- Calcium NaCl: Sodium-Chloride
NCC: Sodium-chloride cotransporter PGE2: Prostaglandin E2
SHEP: Systolic Hypertension in the Elderly
SIADH: Syndrome of inappropriate antidiuretic hormone
References
- Akbari P, Khorasani-Zadeh A (2023) Thiazide Diuretics.
- Hajjar I, Graves JW (2007) Hyponatremia in Older Women. The Journal of Clinical Hypertension. 6(1): 37–39.
- Mori M, Koide T, Imanishi Y, Matsui Y, Matsuda T (2014) Duloxetine-induced hyponatremia in an elderly patient treated with thiazide diuretics. Indian Journal of Pharmacology. 46(6): 657-659.
- Hwang KS, Kim GH (2010) Thiazide-Induced Hyponatremia. Electrolytes & Blood Pressure. 8(1): 51-57.
- Burnier M, Bakris G, Williams B (2019) Redefining diuretics use in hypertension. Journal of Hypertension. 37(8): 1574-1586.
- Ernst ME, Fravel MA (2022) Thiazide and the Thiazide-Like Diuretics: Review of Hydrochlorothiazide, Chlorthalidone, and Indapamide. American Journal of Hypertension. 35(7): 573–586
- Egom, EEA, Wong KYK, Clark AL (2011) Life-threatening hyponatraemia. BMJ Case Reports. 2011.
- AJKDblog (2020) Unraveling Thiazide-Associated Hyponatremia. AJKD Blog.
- Moritz ML, Kalantar-Zadeh K, Ayus JC (2013) Ecstacy- associated hyponatremia: why are women at risk? Nephrology Dialysis Transplantation. 28(9): 2206–2209.
- Sladek CD, Somponpun SJ (2008) Estrogen receptors: Their roles in regulation of vasopressin release for maintenance of fluid and electrolyte homeostasis. Frontiers in Neuroendocrinology. 29(1): 114–127.
- Glover M, Clayton J (2012) Thiazide-Induced Hyponatraemia: Epidemiology and Clues to Pathogenesis. Cardiovascular Therapeutics. 30(5): e219–26.
- UpToDate.(n.d.).www.uptodate.com.https://www.uptodate.com/ contents/diuretic-induced-hyponatremia
- Spigset O, Hedenmalm K (1995) Hyponatraemia and the Syndrome of Inappropriate Antidiuretic Hormone Secretion (SIADH) Induced by Psychotropic Drugs. Drug Safety. 12(3): 209–25.