Adam Martorana, OMS II, Briley Guarneri, OMS II, Ishan Gujral, OMS II, Logan Morrison, OMS II, James F. Keane, DO, Med, Leonard B. Goldstein, DDS, PhD*
A.T. Still University – School of Osteopathic Medicine Arizona
*Corresponding Author: Leonard B. Goldstein, DDS, PhD, A.T. Still University – School of Osteopathic Medicine Arizona, USA
Introduction
E-Sports is a form of sport competition where electronic systems facilitate the primary aspects of the sport; the input of players and teams, as well as the output of the e-sport system, are mediated by human-computer interference [1]. While e-sports can be considered sedentary due to the lack of bodily movement, they may impose significant demands on the body due to rapid and continuous movements of the fingers and concentration demands [2]. E-sport athletes train for 5-10 hours days prior to the competition. It is unclear how such high work demands may affect musculoskeletal pain in E- sports athletes and, subsequently, their performance.
Forward head posture and flexed posture (slouched posture) are frequently observed musculoskeletal consequences of extended exposure to visual display terminals (e.g., Desktop computer, Laptop, Tablet, Smartphone, etc.).
Rapid movements during VR Gaming can lead to injuries. In addition to rapid movements, there is also the additional weight of VR headsets (460-610 grams). A recent study of college e-sport athletes found that 41 % suffered from back and neck pain, and 36 % reported wrist pain. This article will focus on carpal tunnel syndrome (CTS). Since musculoskeletal pain is associated with the utilization of healthcare services, analgesics, and sleep deprivation, these findings should warrant more extensive studies regarding this emerging sport [3,4].
Prevalence of CTS Among E-sport Athletes Due to E-sports research recently becoming an area of research expansion, articles specific to CTS relevant to electronic gaming or competitions are scarce. In order to estimate prevalence, several articles were found that contained the prevalence of CTS or wrist pathologies related to electronic device usage; however, articles were selected to encompass participants over 18 years of age due to 79 % of gamers being in this category [5].
A study found that university individuals using an information and communication device (ICT), including smartphones, personal computers, and gaming consoles, for over 5 hours daily were more likely to develop hand disorders. When referencing time on a gaming console, 49 % of participants who spent at least 2.7 hours on their consoles were found to have a positive Phalen's test, indicating CTS. The study concluded that intensive ICT for more than 5 hours a day is associated with hand disorders and that limiting ICT reduces the risk of developing such disorders6.
A study of 24 university students found that among those who used electronic devices for an average of 9 hours a day, 91.7 % of them experienced upper limb discomfort. More specifically, 45 % of the participants stated hand/wrist pain as their primary source of discomfort. Furthermore, the article noted a strong correlation between repetitive hand movements and carpal tunnel syndrome [7]. Although limited by study selection and size of samples, a correlation can be drawn between repetitive or intensive electronic use for extended periods (> 5 hours) and a higher risk of CTS or wrist pathology development. Thus, a correlation exists between E-sport athletes who train for 5-10 hours daily having a higher risk of developing wrist pathologies
Carpal Tunnel Anatomy
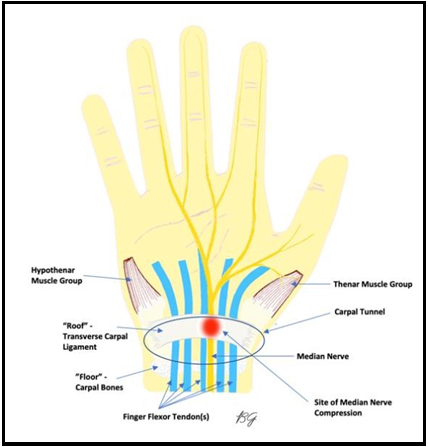
The carpal tunnel is the anatomic passageway from the wrist to the hand found in the proximal wrist on the palmar side. The "floor" of the carpal tunnel comprises the carpal bones, including the pisiform, the hook of the hamate, the scaphoid, and the trapezium. The "roof" of the tunnel is formed by a thick connective tissue called the transverse carpal ligament, also referred to as the flexor retinaculum [8]. The floor and the roof combination create the passageway in which the flexor tendons (flexor digitorum profundus, flexor digitorum superficialis, and flexor pollicis longus) and median nerve travel through in order to reach the hand [8,9]. The median nerve is one of the five terminal branches of the brachial plexus originating from the anterior rami of C5-T19. The median nerve provides sensory perception and motor control to the anterior compartment of the forearm and hand through various terminal branches. The portion of the median nerve traveling through the carpal tunnel eventually gives off 2 significant branches of note in CTS: the recurrent motor branch of the median nerve and the digital cutaneous branch of the median nerve. The recurrent motor branch provides motor innervation to the muscles of the thenar eminence (abductor pollicis brevis, opponens pollicis, and the superficial head of the flexor pollicis brevis) [8,9]. The digital cutaneous branch provides sensory innervation to the palmar surface of the thumb, index, middle and radial half of the fourth digit [9].
Image by Briley Guarneri OMS-2
Mechanism of Injury
Proper anatomic understanding of the carpal tunnel is of utmost importance when evaluating patients with complaints of hand and wrist pain and concomitant paresthesia. CTS occurs when the flexor tendon sheaths swell, or the flexor retinaculum becomes inflamed and causes an increased tunnel pressure compressing the median nerve [10]. The exact mechanism for injury leading to median nerve compression remains an area of speculation, and as such, CTS is described as an idiopathic condition with many known and studied risk factors [11]. Risk factors include female sex, trauma, repetitive wrist movements, and occupation [12].
Furthermore, various conditions can increase inflammation and pressure within the carpal tunnel leading to entrapment of the median nerve. Conditions such as diabetes and rheumatoid arthritis, amongst others, may affect the synovial fluid within the carpal tunnel, effectively increasing the likelihood of developing CTS compared to a healthy individual [13].
Signs/Symptoms
Understanding the signs and symptoms of a typical presentation of CTS is essential for subsequent diagnosis. Typical patient presentation of CTS is associated with the innervation of the median nerve. Specifically, pain and dysesthesia of the ring finger's lateral three digits and lateral half are seen in those with new-onset CTS [8]. In both the absence or presence of pain, a tingling sensation of these digits can be experienced by the patient. In advanced cases of CTS, wasting of the thenar muscles can be seen as well as pain that radiates up the forearm sometimes as far as the shoulder [12]. Associated symptoms of thenar wasting due to CTS include reduced dexterity in day-to-day tasks and a lack of grip strength [8,12]. Therefore inquiring about the patient occupation and lifestyle is essential to understanding the signs and symptoms of CTS.
Clinical diagnosis
Diagnosis of CTS typically involves using various tests that aim to reproduce symptoms seen in CTS. Phalen's, Tinel's, and Durkan's Tests are three commonly used baseline tests used by physicians [10,12]. Phalen's test measures symptoms when the wrist is placed in passive flexion for 60 seconds. These symptoms include pain and dysesthesia of the previously mentioned areas of median nerve innervation. In order to increase flexion of the wrist, both wrists can be passively flexed against one another [12]. Tinel's test involves the physician using either their index or middle finger to firmly tap along the course of the median nerve slightly proximal to the wrist to reproduce symptoms consistent with CTS [10,12]. Another test that can diagnose CTS is the Durkan compression test, in which the physician places three fingers along the course of the median nerve over the carpal tunnel and observes whether pain, tingling, or numbness ensues, indicating CTS. In more advanced cases of CTS, strength testing of the lateral 3.5 digits can be performed to test for thenar muscle wasting and atrophy [12].
The utility of electrophysiological testing in concert with the previously stated clinical tests is often debated, as Phalen's test is both sensitive and specific for CTS (0.94 and 0.96, respectively). In most scenarios, electrophysiological testing is used as confirmatory testing for the diagnosis of CTS or post-surgically to understand changes in nerve conduction and pain and dysesthesia [12]. In conclusion, essential clinical examination by a physician in the absence of atypical symptoms or trauma to the upper limb is deemed sufficient to diagnose CTS [10,12].
Treatment
Standard treatment of CTS currently begins conservatively with rest, immobilization with neutral angle wrist splinting, and non-steroidal anti-inflammatory drugs (NSAIDs). Neutral-angle wrist splinting has offered patients a 37 % success rate in CTS management, and conservative therapies, in general, have shown effectiveness in up to 80 % of patients [14,15]. Local anesthetics and corticosteroid injections are pursued if CTS relapses, or conservative treatments are ineffective. While initial corticosteroid injections have shown between a 53 % to 73 % improvement in CTS, there are frequently noted relapses [14,16] An analysis of wrist splinting versus steroid injection used the Boston Carpal Tunnel Syndrome Questionnaire (BCTQ), which is a patient-based outcome measure of symptom severity and functional status in patients with carpal tunnel syndrome, found significant improvements on BCTQ scores for both the splinting and steroid groups. In comparison, only the steroid group improved the finger dexterity test, better patient satisfaction, and less painkiller use without causing more side effects [16]. Ultimately, the definitive treatment of CTS is the surgical intervention of the TCL to expand the carpal tunnel volume, but it should be reserved for those severe cases [17]
Physical Rehabilitation
There is no established algorithm for the use of physical therapy in patients with CTS. A 2020 study sought to find the optimal combination of physical factors and kinesiotherapy involving therapy with heat, laser, ultrasound, magnetotherapy, iontophoresis, acupuncture, shockwaves, immobilization, and kinesiotherapy. Each therapy has an individual benefit for CTS rehabilitation. However, much research is still needed to develop a standardization of care. Thus, it was recommended that individual rehabilitation programs be created case-to-case basis [18]. While further research is needed in forming CTS treatment algorithms, the benefits of physical therapy have been strongly supported. A study analyzing the effects of physical therapy versus surgical intervention at 4-year follow-up regarding metrics of functional status, symptom severity, self-perceived improvement, and rate of surgical intervention showed no between-group differences in any category. This study suggests that those with CTS may find similar improvement from conservative treatment as they would surgery [19].
Osteopathic Manipulative Medicine
Osteopathic manipulative treatment (OMT) is valuable as a non-invasive diagnostic technique not included in the current standard treatment of CTS. OMT can release the pressure in the carpal tunnel, stretch soft tissues, mobilize restricted metacarpal bones, increase the length of the transverse carpal ligament, improve ROM, strengthen muscles, remove fluid and inflammation, and improve circulation and nerve conduction [15]. A 2015 study utilizing the BCTQ showed statistically significant improvements in symptoms and functions after six weeks of OMT. Further results yielded statistically significant data in the self-reported improvement of symptoms on the treated side, increased length of the transverse carpal ligament, and a significant drop in sensory symptom diagram (SSD) scores after six weeks. However, median nerve function and cross-section had no significant change [20]. Carpal bone mobilization has also significantly decreased a patient's pain rating on the Kruskal-Wallis Test [17].
The approach of osteopathic manipulative treatment is a conservative approach that targets bone, ligament, tendon, nervous system, soft tissue, and the dynamic interaction of structures within a given space leading to improvements of pathologies in general by returning standard structure and function to the area. OMT also helps to monitor the progression of CTS and can minimize repeat imaging, steroidal injections, and surgical intervention leading to lower medical costs for E-sports athletes, which may improve the percentage of athletes who seek treatment [21,22].
Several techniques can be used to treat somatic dysfunction in the wrist and hand that are associated with CTS [22]:
- Wrist Retinaculum - Myofascial Release Thenar and Carpal Ligaments - Opponens Roll Maneuver
- Carpal Bone - HVLA (mobilization with impulse)
- Metacarpophalangeal Joint – HVLA (mobilization with impulse)
- Carpometacarpal Joint – HVLA (mobilization with impulse)
- Radius and Ulna – HVLA (mobilization with impulse) for posterior radial head pronation dysfunction. Muscle Energy Techniques for pronation and supination dysfunctions.
- Interosseous Membrane and Forearm Muscles – Myofascial Release (bilateral thumb pressure technique)
Practical Takeaways
Medical research exploring conditions related to E-Sports gaming is rapidly developing. Utilizing data for CTS in related fields similar to gaming can allow for an accurate diagnosis and treatment plan to be developed for E-sport athletes. Correct recognition of the signs, symptoms, and physical exam related to CTS will allow healthcare professionals to quickly and accurately make a diagnosis without invasive testing or multiple specialty visits [10,22]. This will yield lower healthcare costs, improve patient outcomes and reduce the patient load on medical professionals [12,13,23]. Furthermore, prompt diagnosis ensures chronic changes to the median nerve are not sustained by patients [7].
It should be noted that an over-diagnosis of E-sports-related CTS cases is seen when the diagnosis is made by medical professionals unfamiliar with E-sports ergonomics [3]. Additionally, CTS may not be diagnosed in high prevalence due to a lack of seeking medical attention in general [24]. To address these gaps, clinicians should become familiar with E-sports gaming ergonomics and its relationship to CTS and other injuries.
As previously outlined, conservative therapies remain paramount in CTS due to their effectiveness. In addition to standard rest, immobilization with neutral angle wrist splinting, and NSAIDs, OMT should be supplemented due to its positive results and ability to be immediately implemented in the office [22]. Beyond conservative treatment and OMT, physical therapy can be utilized on a case-by-case basis [18]. Finally, relapsing CTS or ineffective conservative treatment can be treated using local anesthetics or corticosteroid injections and, ultimately, surgical intervention if necessary [19].
Due to the rapid development of E-Sports, the primary goals remain prevention and patient education. Players should be instructed on proper ergonomics to reduce repetitive motions and limit the prolonged sitting time when possible. more, players should be instructed to contact medical professionals upon the appearance of symptoms to aid in prompt diagnosis and an appropriate treatment regimen. Clinicians should be educated on the demands required of E-Sport athletes in order to provide quick and accurate diagnos is and treatment. Lastly, as other sports require physical examinations to compete, a protocol should be implemented to help raise awareness of joint injuries related to E-sports and the proper steps to take when one begins to experience symptoms related to an injury.
References
- Hamari J, Sjöblom M (2017) What is eSports and why do people watch it? Internet Res. 27(2): 211-232.
- Schaeperkoetter CC, Mays J, Hyland ST, Wilkerson Z, Oja B, et al. (2017) The “New” Student-Athlete: An Exploratory Examination of Scholarship eSports Players. J Intercoll Sport. 10(1): 1-21.
- Difrancisco-Donoghue J, Balentine J, Schmidt G, Zwibel H (2019) Managing the health of the eSport athlete: An integrated health management model. BMJ Open Sport Exerc Med. 5(1).
- Rathleff MS, Holden S, Straszek CL, Olesen JL, Jensen MB, et al. (2019) Five-year prognosis and impact of adolescent knee pain: a prospective population-based cohort study of 504 adolescents in Denmark. BMJ Open. 9(5): 24113.
- Kowal M, Conroy E, Ramsbottom N, Smithies T, Toth A, et al. (2021) Gaming your mental health: A narrative review on mitigating symptoms of depression and anxiety using commercial video games. JMIR Serious Games. 9(2): 1-13.
- Saito K, Saito Y (2021) Relationship between Information and Communication Device Usage and Development of Hand Disorders. Inq (United States). 58: 469580211029607.
- Woo EHC, White P, Lai CWK (2019) Morphological Changes of the Median Nerve Within the Carpal Tunnel During Various Finger and Wrist Positions: An Analysis of Intensive and Nonintensive Electronic Device Users. J Hand Surg Am. 44(7): 610.e1-610.e15.
- Newington L, Harris EC, Walker-Bone K (2015) Carpal tunnel syndrome and work. Best Pract Res Clin Rheumatol. 29(3): 440-453.
- Davis DD, Kane SM (2022) Median Nerve Palsy - StatPearls - NCBI Bookshelf. Published 2021.
- Wipperman J, Goerl K (2016) Carpal Tunnel Syndrome: Diagnosis and Management. Am Fam Physician. 94(12): 993- 999.
- Genova A, Dix O, Saefan A, Thakur M, Hassan A (2020) Carpal tunnel syndrome: a review of literature. Cureus. 12(3): e7333.
- Middleton SD, Anakwe RE (2014) Carpal tunnel syndrome. BMJ. 349: g6437.
- Zamborsky R, Kokavec M, Simko L, Bohac M (2017) Carpal tunnel syndrome: Symptoms, causes and treatment options. A literature reviev. Ortop Traumatol Rehabil. 19(1): 1-8.
- Bland JDP (2007) Treatment of carpal tunnel syndrome. Muscle and Nerve. 36(2): 167-171.
- Sucher BM (2012) Osteopathic manipulative medicine for carpal tunnel syndrome. J Am Osteopath Assoc. 112(6): 383-384.
- Dammers JWHH, Roos Y, Veering MM, Vermeulen M (2006) Injection with methylprednisolone in patients with the carpal tunnel syndrome. J Neurol. 253(5): 574-577.
- So H, Chung VCH, Cheng JCK, Yip RML (2018) Local steroid injection versus wrist splinting for carpal tunnel syndrome: A randomized clinical trial. Int J Rheum Dis. 21(1): 102-107.
- Zaralieva A, Georgiev GP, Karabinov V, Iliev A, Aleksiev A (2020) Physical Therapy and Rehabilitation Approaches in Patients with Carpal Tunnel Syndrome. Cureus. 12(3): e7171.
- Fernández-De-Las-Peñas C, Arias-Buría JL, Cleland JA, Pareja JA, Plaza-Manzano G, et al. (2020) Manual therapy versus surgery for carpal tunnel syndrome: 4-year follow-up from a randomized controlled trial. Phys Ther. 100(11): 1987-1996.
- Tal-Akabi A, Rushton A (2000) An investigation to compare the effectiveness of carpal bone mobilisation and neurodynamic mobilisation as methods of treatment for carpal tunnel syndrome. Man Ther. 5(4): 214-222.
- Amadio PC (1992) The Mayo Clinic and Carpal Tunnel Syndrome. Mayo Clin Proc. 67(1): 42-48.
- Burnham T, Higgins DC, Burnham RS, Heath DM (2015) Effectiveness of osteopathic manipulative treatment for carpal tunnel syndrome: A pilot project. J Am Osteopath Assoc. 115(3): 138-148.
- Gunnarsson LG, Amilon A, Hellstrand P, Leissner P, Philipson L (1997) The diagnosis of carpal tunnel syndrome: Sensitivity and specificity of some clinical and electrophysiological tests. J Hand Surg Eur Vol. 22(1): 34-37.
- Hwu M. 1HP 2020 Year in Review: Esports Medicine & Performance Team - 1-HP.