Amit Mandal*, Oommen K George
Department of Cardiology, Christian Medical College, Vellore, Tamil Nadu, India
*Corresponding Author: Amit Mandal, Department of Cardiology, Christian Medical College, Vellore, Tamil Nadu, India.
Abstract
A sinus of Valsalva aneurysm (SVA) is a rare cardiac anomaly. Presentation varies from asymptomatic findings to acute heart failure, which can rapidly worsen to cause death.
Although surgery is the gold standard treatment, percutaneous transcatheter closure has now become equally efficacious with fewer complications. Here, we present a case of an 18-year-old woman with an acute rupture of an SVA into the RVOT with significant shunting from RCC to RVOT who underwent transfemoral RSOV device closure.
Keywords: Sinus of Valsalva, Aneurysm, Congenital heart disease
Introduction
Background
A sinus of Valsalva aneurysm (SVA) is a rare cardiac anomaly which could be congenital or acquired. Aneurysms of the sinus of Valsalva are typically more common in men (4:1) and there is a higher incidence in Asian populations. [1] An SVA is a consequence of the weakness of the elastic lamina at the junction of the aortic media and the annulus fibrosis [2]. A congenital SVA is usually clinically silent but may vary from a mild, asymptomatic dilation detected in routine two-dimensional echocardiography to symptomatic presentations related to the compression of adjacent structures or intracardiac shunting caused by rupture of the SVA into the right side of the heart. Approximately 65–85% of SVAs originate from the right sinus of Valsalva, while SVAs originating from non-coronary (10–30%) and left sinuses (< 5%) are exceedingly rare. [3] Here, we present a case of a 18-year-old woman with an acute rupture of an SVA into the RVOT with significant shunting from RCC to RVOT who underwent transfemoral RSOV device closure.
Case presentation
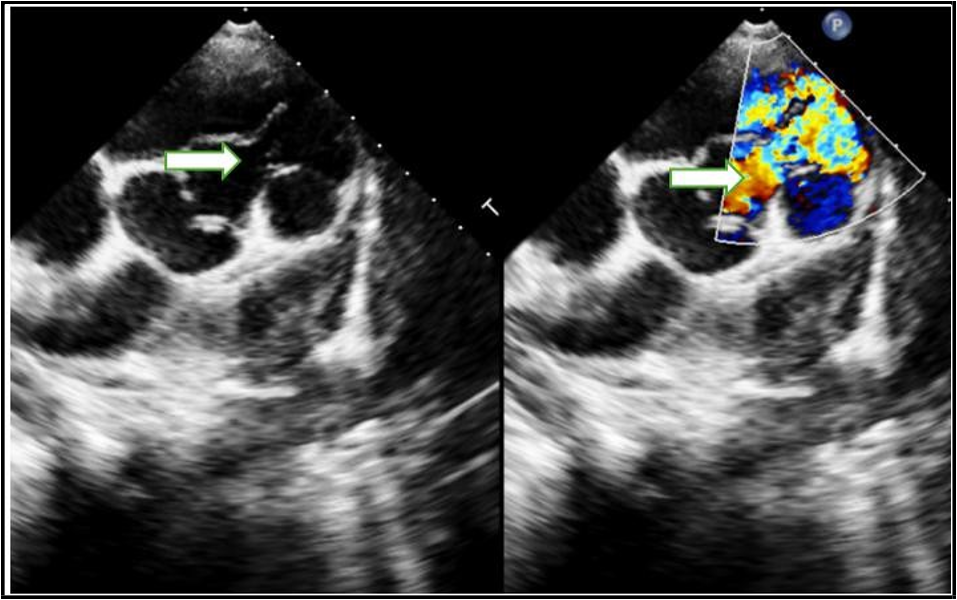
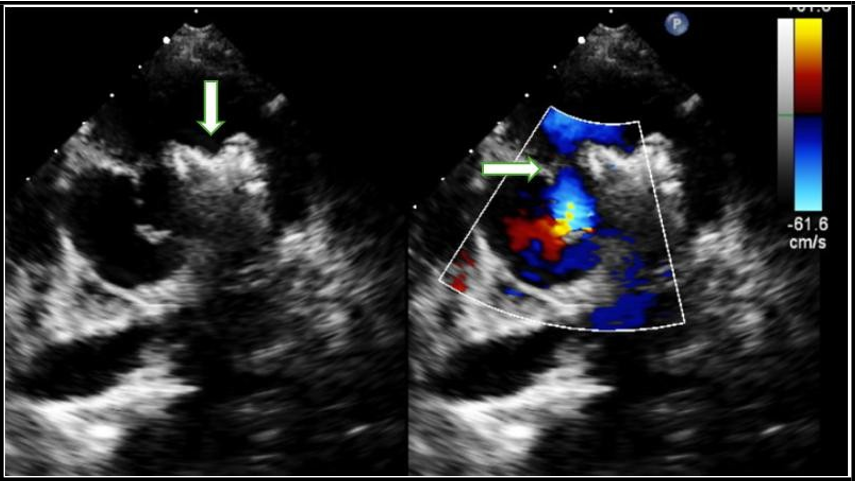
An 18-year-old lady presented with a history of intermittent dyspnoea on exertion associated with exertional palpitations of 10 months duration. There was no history of chest pain or syncope. There was no history of prolonged fever or cerebrovascular accident in the past. Her vital signs included a blood pressure of 110/ 70 mmHg with a pulse rate of 90 beats per minute, a respiratory rate of 16 per minute and oxygen saturation of 98% on room air. Further examination demonstrated a continuous machinery cardiac murmur best heard at the left parasternal border, loudest in systole (5/6), with a palpable thrill across the precordium. There was no relevant past medical history or significant family history. Electrocardiogram (ECG) showed sinus rhythm, no significant ST-T changes. Transthoracic echocardiography (TTE) was subsequently performed for investigation of the new continuous murmur – other differentials other than a SVA considered were patent ductus arteriosus, coarctation of the aorta, coronary arteriovenous fistulas and an aortopulmonary window. TTE showed normal left and right ventricular size and systolic function. It also showed RSOV (rupture sinus of Valsalva) measuring about 7mm with a shunt from RCC to RVOT and continuous flow noted across the defect (Figure 1). She was admitted for closure of the same and she underwent transfemoral RSOV device closure.
Procedure details Access:
RFA-5F short sheath
RFV-6F short sheath--10F 75 cm contralateral sheath
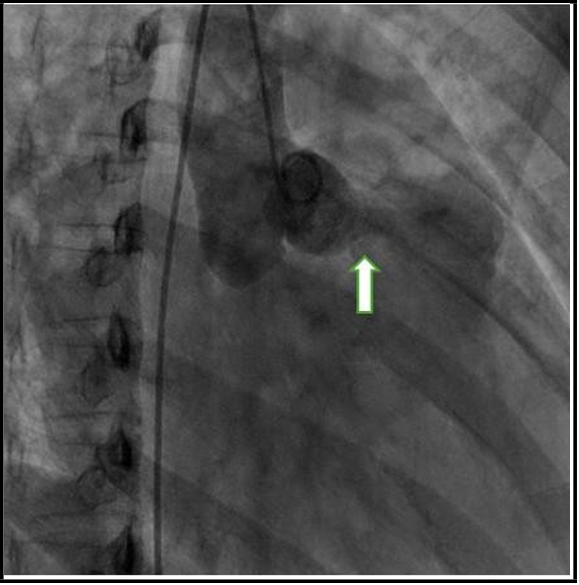
Initial angiogram with pigtail in aortic root measured RSOV to be 9.5mm. (Figure 2) The RSOV was crossed from the aorta into the RVOT using a 6F JR diagnostic catheter with glidewire and was advanced into IVC (Via RVOT--RV--RA--IVC). The glide wire was snared out from the right femoral venous approach using a 6F 20 cm loop goose neck snare and exteriorised. A 10F 75 cm sheath was tracked over this wire with its distal end in the ascending aorta. A 18/16 (Lifetech PDA device) was backloaded onto the 75 cm long sheath using a short 9F sheath. The device was positioned in the cul- de-sac of the sinus of valsalva aneurysm.
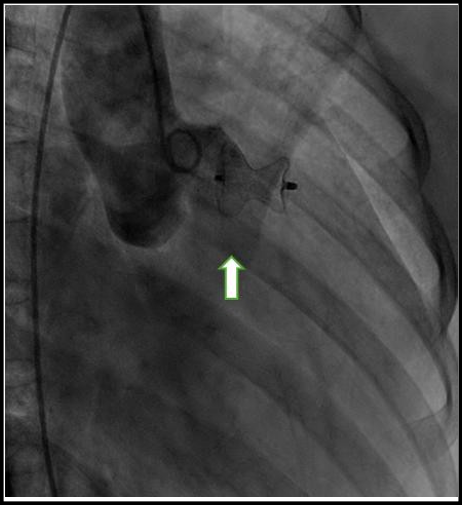
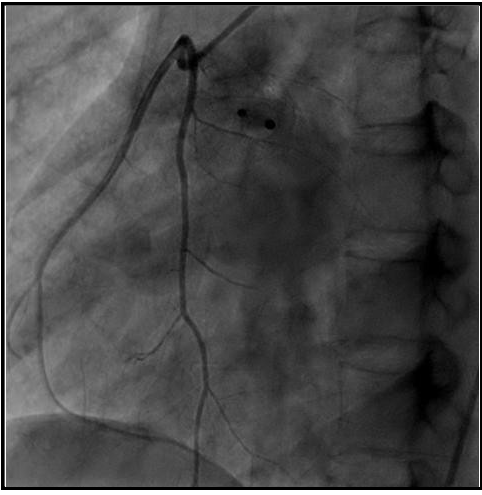
The position of the device was ascertained under fluoroscopy and the transthoracic echocardiogram. Aortogram confirmed adequate position and the device was deployed. (Figure 3) Post deployment angiogram revealed fair result with trivial flow through the device and no significant worsening of aortic regurgitation. Patient remained hemodynamically stable throughout the procedure. Final selective check angiogram of RCA showed no involvement of RCA ostium as its origin was away from device site higher up from sinotubular junction. (Figure 4) Post procedure transthoracic echocardiography showed device in situ and small residual shunt across RSOV. (Figure 5) Post-procedure hospital stay was uneventful, and she was hemodynamically stable at discharge. At one year, two year and three years follow up she remained asymptomatic with no worsening of residual shunt.
Figure 1: TTE showing RSOV measuring about 7mm with shunt from RCC to RVOT, (white arrow), continuous flow was noted across the defect
Figure 2: Angiogram with pigtail in aortic root showing RSOV (white arrow)
Figure 3: Deployment of Lifetech PDA device in the sinus of valsalva aneurysm
Figure 4: Selective check angiogram of RCA showing no involvement of RCA ostium
Figure 5: Transthoracic echocardiography showing device in situ (white arrow) and small residual shunt across RSOV (white arrow).
Discussion
Performing the TCC of RSOV rather than surgical treatment has been dramatically favoured since its introduction in 1994. However, a comprehensive guideline on the indications, patient selection, choice of imaging modalities, device selection, and complication prevention is still lacking.[4] Since the first reported case of the TCC of RSOV in 1994, mounting evidence (mostly case reports and a small number of case series) has indicated the effectiveness of TCC as a potential alternative to surgical intervention.
Patient selection for Transcatheter closure (TCC)
Precise patient selection criteria are critical before TCC. Xiao et al. [5] considered patients to have TCC if they have a body weight exceeding 10 kg, if the non-coronary sinus or the right coronary sinus is the origin of the defect rupturing into the right ventricle or the right atrium, if the defect size is less than 10 mm, if RSOV does not affect the aortic valve and has more than a 7 mm distance from the annulus of the aortic valve, if a gap of more than 5 mm exists between the ostium of the right coronary sinus and the ruptured site, and if surgery is needed in the absence of other cardiac anomalies.
Lui et al. [6] also suggested that RSOV patients with a European System for Cardiac Operative Risk Evaluation II (EuroSCORE II) score exceeding 20% would benefit from TCC. Nevertheless, controversy remains over the indications for TCC in patients with RSOV since this method is new and the prevalence of RSOV is low. Further studies are, therefore, required to validate the indications or contraindications of TCC in patients with RSOV[7]
Transcatheter occluder devices
The first case of the TCC of RSOV was performed utilizing a Rashkind Umbrella via an arterial approach [4]. However, the transvenous approach has been performed more frequently because of its higher maneuverability and easier access to the Valsalva sinus. Recent decades have seen the use of other devices, including Amplatzer ductal occluders, PDA occluders, muscular ventricular septal defect occluders, septal occluders, and coils, depending on the anatomy of the defect. Amplatzer-type ductal occluder devices have been in frequent use due to the conformity of their shape with RSOV morphology [8]. Other than the characteristics of the defect, the interventionist’s familiarity with the device, the availability of the device, and financial concerns are taken into consideration in device selection.
Complications
Although shown to be effective, the TCC of RSOV can be associated with severe complications on rare occasions. The new onset or progression of an existing aortic regurgitation is the most critical complication in the TCC of RSOV. Aortic insufficiency can be due to traction on the aortic valve annulus or an aortic valve injury during the procedure. In cases of severe aortic insufficiency, surgical intervention is unavoidable. Compression of the coronary arteries after device insertion can also be a life-threatening complication, which can be avoided by visualizing coronary artery flow during the intervention via angiography. A new onset of ST depression after device implantation can also be due to coronary artery compression. If left undetected, the condition could cause myocardial infarction [9] Embolization of the occluder device can also be a possible complication. Hemolysis is also a rare complication of TCC caused by the inserted device [10]. In rare situations, disturbances in the conduction pathways might result in arrhythmias, including atrioventricular or bundle branch blocks. These blocks are caused by possible traction or compressions on conductive pathways. As with any percutaneous intervention, complications associated with catheterization sites, including atrioventricular fistulae, hematoma, and bleeding events, are also possible. Our patient did not develop any peri-procedural complications.
Learning points
1. Ruptured sinus of Valsalva aneurysm is a rare cardiac anomaly.
2. Presentation varies from asymptomatic findings to acute heart failure, which can rapidly worsen to cause death.
3. Physical examination is invaluable in patient assessment - a new continuous murmur is always significant and must prompt urgent echocardiography to facilitate timely diagnosis and treatment.
4. Although surgery is the gold standard treatment, percutaneous transcatheter closure has now become equally efficacious with fewer complications.
Ethics approval
The patient's father provided written informed consent to be published as a case report.
Acknowledgments: Thanks to the patient and his family for the informed consent
Competing interests: No conflict of interest is to be declared by the authors.
Funding: This study received no external funding.
References
- Feldman DN, Roman MJ (2006) Aneurysms of the Sinuses of Valsalva. Cardiology. 106(2): 73-81.
- Weinreich M, Yu P-J, Trost B (2015) Sinus of Valsalva Aneurysms: Review of the Literature and an Update on Management. Clinical Cardiology. 38(3): 185-189.
- Mahajan K, Asotra S, Negi P, Merwaha R (2015) Successful device closure of a ruptured sinus of Valsalva aneurysm presenting with acute heart failure. Case Rep. 2015: bcr2015212883.
- Ayati A, Toofaninejad N, Hosseinsabet A, Mohammadi F, Hosseini K (2023) Transcatheter closure of a ruptured sinus of valsalva: a systematic review of the literature. Front Cardiovasc Med. 10: 1227761.
- Xiao JW, Wang QG, Zhang DZ, Cui CS, Han X, et al. (2018) Clinical outcomes of percutaneous or surgical closure of ruptured sinus of Valsalva aneurysm. Congenit Heart Dis. 13(2): 305–10.
- Liu S, Xu X, Zhao X, Chen F, Bai Y, et al. (2014) Percutaneous closure of ruptured sinus of Valsalva aneurysm: results from a multicentre experience. EuroIntervention. 10(4): 505–12.
- Yang K, Luo X, Tang Y, Hu H, Sun H (2021) Comparison of clinical results between percutaneous closure and surgical repair of ruptured sinus of Valsalva aneurysm. Catheter Cardiovasc Interv. 97(3): E354–E361.
- Al-Senaidi KS, Al-Farqani A, Maddali M, Al-Maskary S (2016) Transcatheter Closure of Ruptured Sinus of Valsalva Aneurysm: Report of two cases. Sultan Qaboos Univ Med J. 16(4): e511- e515.
- Bolen MA, Popovic ZB, Tandon N, Flamm SD, Schoenhagen P, et al. (2012) Image Quality, Contrast Enhancement, and Radiation Dose of ECG-Triggered High-Pitch CT Versus Non–ECG- Triggered Standard-Pitch CT of the Thoracoabdominal Aorta. Am J Roentgenol. 198(4): 931–8.
- Cullen S, Somerville J, Redington A (1994) Transcatheter closure of a ruptured aneurysm of the sinus of Valsalva. Br Heart J. 71(5): 479–80.