Aviral Vij MD1, Lolita Golemi 1, Christina Anderson MD1, Steve Attanasio DO1, *
1 Division of Cardiology, RUSH University Medical Center, Chicago, IL
*Corresponding Author: Steve Attanasio DO, Division of Cardiology, RUSH University Medical Center, Chicago, IL.
Abstract
Coronavirus Disease of 2019 is a highly transmissible and sometimes fatal infection caused by the SARS-CoV-2 virus. We present two patients with sub-massive pulmonary embolism in the setting of inactivity while in “self-quarantine” and reinforce the advice from the World Health Organization about measures to stay physically active while at home.
Keywords: COVID-19, Pulmonary Embolism, Inactivity, self-quarantine, Pulmonary embolism response team, catheter-directed thrombolysis, aspiration thrombectomy
Abbreviations: COVID-19: Coronavirus disease of 2019; WHO: World health organization; CDC: Center for disease control; VTE: Venous thromboembolism; EKG: Electrocardiogram; CTA: Computed tomography angiography; TTE: Transthoracic echocardiogram; DVT: Deep vein thrombosis; RV: Right ventricle; LV: Left ventricle
Introduction
Coronavirus Disease of 2019 (COVID-19) is a highly transmissible and often fatal infection caused by SARS-CoV-2 virus. Given its aggressive expansion and transmission, COVID-19 was labeled a pandemic by the World Health Organization (WHO) on March 11, 2020 [1]. Poor disease understanding and lack of preparedness has contributed to the spread with now over 8.9 million cases worldwide and around 2.2 million cases in the United States with 183,000 deaths (US), per CDC as of August 27, 2020.[2]
In the absence of a prophylactic vaccine and to mitigate disease transmission, several states have passed “shelter-in-place” orders to minimize the person-to-person spread and prevent transmission amplification events. Self-quarantining can lead to lifestyle changes that pose a significant challenge to staying physically active.
Although the importance of maintaining an active lifestyle during confinement is widely acknowledged, adhering to such recommendations has not been easily attainable for everyone. Patients at risk for venous thromboembolism (VTE) under normal circumstances such as those with prior VTE, obesity, use of oral contraceptive pills and malignancy remain at the greatest risk for suffering adverse thromboembolic events during this time. Additional efforts to educate and promote physical activity in these patients are warranted.
Here, we want to highlight two cases of patients with pre-existing risk factors for VTE who presented to the hospital during the self- quarantining period with sub-massive pulmonary embolism (PE) and discuss the treatment considerations.
Patient 1:
History of presenting illness:
A 52-year-old man with obesity (BMI: 38kg/m2) presented to the Emergency department (ED) with sudden onset of shortness of breath followed by a syncopal episode. The patient had been strictly adhering to the shelter-in-place guidelines and consequently limited his physical activity. He reported a prolonged duration of sitting for up to 10 hours a day for the last 7-10 days.
Vitals and physical examination:
He was noted to be tachypneic with a respiratory rate (RR) of 32, tachycardia with heart rate (HR) of 127 bpm, and hypoxemic with O2 saturation of 88 % on room air. Blood pressure was initially 107- 138/60-98 mmHg.
Investigations:
COVID-19 PCR testing was negative. Labs showed an elevated brain natriuretic peptide (BNP) of 494 pg/mL (normal <50 pg/mL) and a troponin of 4.24 ng/mL (normal < 0.01 ng/mL). Electrocardiogram (EKG) (Figure 1a) on admission showed evidence of right ventricular strain and an S1Q3T3 pattern and T-wave inversion in leads V1-V3. Computed tomography angiography (CTA) (Figure 1b) demonstrated a saddle embolus extending into bilateral posterior basal and lateral basal segments with Right ventricle (RV): left ventricle (LV) ratio of 1.2. A transthoracic echocardiogram (TTE) (Figure 1c) confirmed acute right heart strain showing a moderately dilated RV with reduced systolic function consistent with “McConnell’s sign” (akinesia of the right ventricular free wall with sparing of the apex). Lower extremity venous dopplers did not show any evidence of deep vein thrombosis (DVT).
Management:
The case was reviewed with the Pulmonary embolism response team (PERT). The patient was started on a heparin drip and underwent bilateral ultrasound-facilitated catheter-assisted thrombolysis (Figure 1d). After a bilateral 12-hour EKOS (Boston Scientific, Marlborough, MA) treatment session, the patient had near-complete resolution of RV strain on TTE and was discharged home on room air and oral anticoagulation.
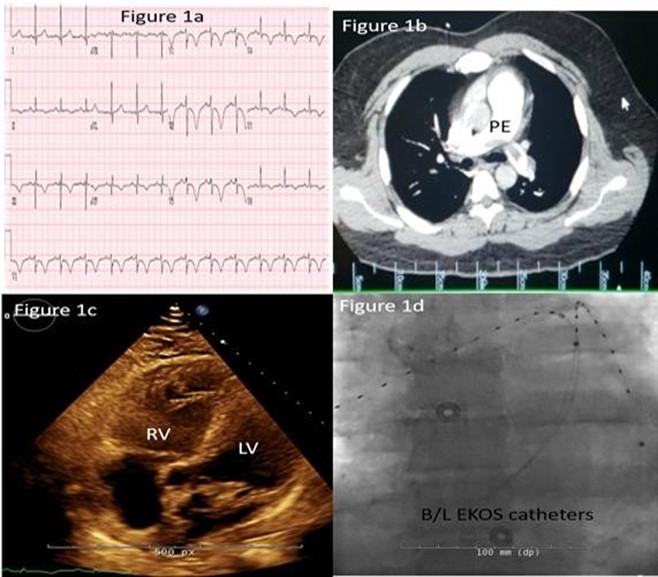
Figure 1a: Electrocardiogram showing evidence of Right ventricular strain (S1Q3T3 pattern).
Figure 1b: Computed tomography angiography showing saddle pulmonary embolism at the bifurcation of main pulmonary artery.
Figure 1c: Echocardiogram showing dilated Right ventricle.
Figure 1d: Bilateral “EKOS catheter” placement for ultrasound facilitated catheter assisted thrombolytics.
Patient 2:
History of presenting illness:
An 18-year-old female with obesity (BMI of 38 kg/m2), on oral contraceptives (norgestimate-Ethinyl estradiol) for the past several years presented to the ED following recurrent syncopal episodes and shortness of breath. She had been more sedentary than usual given the shelter-in-place orders.
Vitals and physical examination:
Upon arrival to the ED, she was tachycardic with HR of 122/min and tachypneic with RR of 24/min. Blood pressure was 94/56 mmHg and initial resting O2 saturation of 97 %.
Investigations:
PCR for SARS-CoV-2 the virus was negative. Her labs were significant for an elevated troponin to 0.20 ng/mL (normal < 0.01 ng/mL) and elevated brain natriuretic peptide (BNP) to 781 pg/mL (normal < 50 pg/mL). EKG (Figure 2a) was significant for right heart strain and prominent S1Q3T3 pattern. CTA (Figure 2b) showed acute pulmonary emboli involving the main pulmonary arteries, with extension into all lobar pulmonary arteries and multiple segmental and subsegmental pulmonary arteries, lingula infarction, and an RV: LV ratio of 1.8. A TTE (Figure 2c) demonstrated “McConnell’s sign” with a marked reduction in RV function. Lower extremity dopplers were negative for DVT.
Management:
The PERT team was consulted and given the high-risk, sub-massive PE with borderline low systolic blood pressure; a decision was made to perform mechanical aspiration thrombectomy. We determined that there was clinical equipoise in choosing an interventional PE strategy and either catheter-directed thrombolysis (CDT) or percutaneous mechanical aspiration thrombectomy would be acceptable treatment options. After a successful mechanical thrombectomy with the T24 FlowTriever system (Inari Medical Inc., Irvine, CA, USA), the patient’s pulmonary arterial pressures improved from 52/23 mmHg (mean: 35 mmHg) to 23/10 mmHg (mean: 16 mmHg) immediately with the extraction of large thrombus burden (Figure 2d) and resolution of RV dysfunction on repeat TTE the next morning. The patient was discharged home without oxygen therapy and on oral anticoagulation 48 hours later.
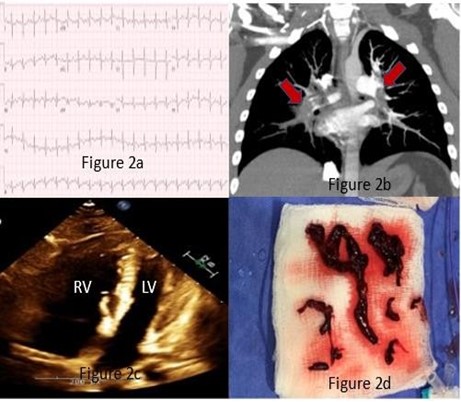
Figure 2a: Electrocardiogram showing Right ventricular strain (S1Q3T3 pattern).
Figure 2b: Computed tomography angiography showing large thrombus burden in bilateral pulmonary arteries.
Figure 2c: Echocardiogram showing dilated Right ventricle.
Figure 2d: Aspirated clot using T24 Inari FlowTriever mechanical aspiration catheter.
Discussion
Venous thromboembolism (VTE) encompasses deep vein thrombosis and pulmonary embolism. VTE remains a significant cause of death in the United States and worldwide, however, PE is rare in adolescents [3]. COVID-19 is associated with a prothrombotic state, increasing the risk for VTE [4], although, as in our patients, physical inactivity by itself in the absence of COVID-19 infection can put patients at significant risk of VTE, especially if they have predisposing risk factors such as obesity, use of oral contraceptives, etc.
With the temporary closure of fitness clubs and public parks, many people do not have access to the usual exercise means. Getting enough physical activity at home can be particularly difficult when shelter-in-place restrictions are in place. The World Health Organization (WHO) recommends at least 150-300 minutes a week of moderate-intensity, or 75-150 minutes a week of vigorous-intensity aerobic physical activity, or an equivalent combination of moderate and vigorous-intensity aerobic activity. Advice from the WHO includes taking short active breaks during the day, following online exercise courses, walking, and engaging in relaxation techniques which can also help manage emotional stress and help maintain optimal mental health [5]. It has been difficult to deliver this message to our patients given the abrupt decrease in routine outpatient visits. Telemedicine has taken on a more prominent role in caring for patients in the outpatient setting and can be used as a platform to reinforce the recommendations to stay active while under quarantine.
Additionally, this case series also highlights the value of a PERT team in managing these patients. Both patients had high-risk sub-massive PE’s (RV strain and elevated biomarkers). There is accumulating evidence that these patients may benefit from more aggressive therapies over anticoagulation alone. However, choosing CDT, systemic thrombolysis, percutaneous mechanical thrombectomy, or surgical thrombectomy should be done using a multidisciplinary approach, usually in the context of a PERT team. There are unique risks and benefits to each treatment modality in PE and a complete review is outside the scope of this case series.
Conclusion
The United States is at the epicenter of both the obesity epidemic and the COVID-19 pandemic. We must urge our patients to maintain adequate physical activity during this period quarantine/shelter in place and perhaps pay closer attention to those with pre-existing risk factors for VTE.
Learning objectives
COVID-19 illness has reached pandemic proportions due to its high transmissibility.
Although we have taken steps to avoid person to person contact and reduce this transmission, this has come at the cost of being physically inactive. Apart from the emotional and mental challenges posed, physical inactivity while in periods of “stay at home” has led to worsening of chronic medical illnesses like hypertension and diabetes, and predisposed patients to development of venous thromboembolism.
Disclosures: There are no disclosures for any of the authors.
Funding: There was no funding for this study.
References
-
Organization WH. WHO Director-General's opening remarks at the media briefing on COVID-19.2020
-
Prevention CDC. Cases of Coronavirus Disease (COVID-19) in the U.S., 2020.
-
Shirakawa T, Iso H, Yamagishi K, Yatsuya H, Tanabe N, et al. (2016) Watching Television and Risk of Mortality From Pulmonary Embolism Among Japanese Men and Women: The JACC Study (Japan Collaborative Cohort). Circulation. 134(4): 355-357.
-
Connors JM, Levy JH (2020) Thromboinflammation and the hypercoagulability of COVID-19. J Thromb Haemost. 18(7): 1559-1561.
-
WHO guideline. “Stay physically active during self-quarantine” (2020).



