Alemayehu Desale Gonfa1*, Lazimu Yasin2, Kemal Jemal3, Lidiya Zerihun4
1Midwifery department, health science college, Mattu University
2Mattu health science college
3,4Nursing department college of health science, salale university
*Corresponding Author: Alemayehu Desale Gonfa, Midwifery department, health science college, Mattu University.
Abstract
Background: Type 2 diabetes mellitus (T2DM) is a leading cause of morbidity and mortality among older adults worldwide, particularly in low-resource countries. Self-care is important for T2DM management by controlling further complications and maintaining the well-being of the patients.
Objective: The aim of this study is to assess self-care practice and associated factors among older adults of T2DM patients who are attending public hospitals in the Buno Bedele zone, Oromia, Ethiopia, 2022.
Methods: Facility-based mixed design was conducted from April 15/2022 to June 20/2022. About 386 T2DM patients were selected using a systematic random sampling for the quantitative and 13 key informants were determined using the purposively sampling technique for the qualitative approach. Pre-tested structured and semi-structured face-to-face interviewer-administered questionnaires and guiding questions were used to collect quantitative and qualitative data, respectively. Data was entered into Epidata version 4.6 and exported to the statistical package of social science version 25 for analysis. Bivariate and multivariable logistic regression was analyzed and significance was approved at p-value <0.05 with 95% confidence intervals for quantitative analysis. Idea saturation and thematic analysis were used for the qualitative approach.
Results: Out of 386 (95.5%) respondents, 174 (45.1%) had good diabetes self-care practice. Favourable attitudes [AOR=2.03; 95% CI: (1.13-3.64)], having complications [AOR=6.56; 95% CI: (3.38-12.77)], having your own glucometer [AOR= 5.78; 95% CI: (2.14-12.52)], family care and support [(AOR= 3.01; 95% CI: (1.68-5.41), and follow-up adherence [AOR=3.84; 95% CI: (1.60-9.19)] were significantly associated with good diabetes self-care practice. Knowledge of DM, good adherence to medication and medical advice, challenges of diabetes self-care practice, self-care benefits, and recognition of diabetes complications were themes that emerged in the qualitative analysis.
Conclusion: The practice of self-care among T2DM patients was low. Family care & support, having your own glucometer, favourable attitudes, appointment adherence, and diabetes complications were positively associated with good diabetes self-care practice, and knowledge of DM, good adherence to medication and medical advice, challenges of diabetes self-care practice, self-care benefits, and recognition of diabetes complications were themes emerged from qualitative finding.
Recommendation: Self-care advice should be continued to improve T2DM self-care practice that reduces the complications of DM.
Keywords: Type 2 DM, Self-care practice, Diabetes, older adults, chronic disease
Introduction
Diabetes mellitus is a common prevalent chronic metabolic disorder characterized by hyperglycemia that develops because of insulin deficiency (type 1 DM), and insulin resistance (type 2DM) [1]. More than 425 million people are affected with DM worldwide which results in approximately 4 million people‘s death per year, and this problem is a more serious public health problem in older adults [2]. The African region had the highest percentage of undiagnosed diabetes, at an estimated 66.7% of all cases of diabetes and Ethiopia is one of the highest diabetes numbers in Africa (1.9 million) [1].
Older persons‘ as all persons over the age of 60 [3]. Type 2 DM is the most common type of diabetes, accounting for 90 to 95 percent of all diabetic patients [4]. Type 2diabetes is a leading cause of morbidity and mortality among older adults, particularly Africans and Africans- Americans [5]. Greater than 134.6 million older adults worldwide have diabetes, and the number is projected to rise above 252.8 million by 2035) [2]. Greater than one-fifth of all diabetes patients are > 60 years of age [6]. Diabetes self-care involves behaviors such as healthy food, regular physical activity, foot care, medication adherence, and self-monitoring blood glucose (SMBG) [7]. The goals of diabetes self-care practice for T2DM are to prevent or delay complications and maintain quality of life [8]. Self-care is believed to play an important role in T2DM management, and glycemic control. Diabetes is a complex and difficult condition that requires daily self-care practice decisions made by diabetic patients and education on diabetes self- care practice so they can confidently handle their everyday self-care routinely to improve their quality of life [8]. Diabetes self-care practice necessitates information, decision-making, and skill mastery [3]. Older adults with diabetes are at higher risk of developing diabetic macrovascular and micro-vascular complications [9]. Formerly, DM has been a disease affecting developed countries however; recently, it became a problem in all populations worldwide, particularly in developing countries [10]. Three-quarters (75%) of people with diabetes were estimated to be living in low- and middle- income countries [1]. Diabetes prevalence peaked at ages 65–69 years for men and ages 75– 79 years for women [1]. The African region had the highest percentage of undiagnosed diabetes, at an estimated 66.7% of all cases of diabetes and Ethiopia is one of the highest diabetes numbers in Africa (1.9 million) [1]. The status of Diabetes self-care practice is still in question and below standard regardless of increasingly emerging health institutions and professionals. A study conducted in Bahir Dar, Northwest Ethiopia (28.4%) [1] and a study done in the central zone of Tigray public Hospitals (37.3%) [11] the status of diabetes self-care practice is very low. Factors associated with diabetes self-care:- education, diabetes complication, diabetes category, distance, and appointment adherence were significantly associated with the DSCP study done in Southern Dawuro Tarecha Hospital [8]. In Ethiopia, diabetes is the most typical reason for admission that hastens development issues such as heart attacks and strokes; as a result, an individual's lifespan is reduced by 10–15 years, despite this, a characteristic of self-care practice behaviors is focused on others [12]. Diabetes Self-care practice addresses the comprehensive issue of clinical, educational, psychosocial, and behavioral aspects of care needed for daily self-care practice and that lays the groundwork for all diabetics to be helped [13]. Although the prevalence of diabetes mellitus is distributed in the different geographical regions of Ethiopia, especially in the Buno-Bedele such studies were limited. The use of diabetic self-care practices could help to reduce diabetes-related complications as well as premature deaths [3]. Self-care practice is become decreasing in older age due to limitation of physical activities, forgetfulness to take prescribed medication, not having regular follow up, and become reducing giving self-care practice and unaware of the need for self-care and how to practice it. Because of these reasons, they are at risk to develop DM complications and co-morbidities. Investigating the prevalence of self-care practice and associated factors among older adults with T2DM is crucial, particularly in the study area. A mixed method study is to get a better understanding of self-care practice among older T2DM patients that can be gained beyond quantitative and qualitative results and to reach the optimum threshold to resolve the gap.
This study was designed to assess the level of self-care practice and associated factors among T2DM older adults visiting the Public Hospitals of Buno-Bedele Zone.
Thus, it is expected that the result of this study will guide nurse educators, counselors, and adherence supporters in diabetic self-care practice adherence related education. The findings from this study will also improve awareness of patients, pharmacists, and nurses related to older adults‘ self-care practice. In addition, this study will also help nurses to educate the patients on the importance of self-care practice and reduce the early development of diabetic complications. It is also expected that the finding from this study may help in designing a future nursing educational plan for older patients having self-care practice improved quality of life, reduced morbidity, and mortality from diabetes mellitus. This study's findings might also help provide baseline data for researchers who want to conduct further studies on a similar topic.
Objectives General Objective
Assessing self-care practice and associated factors among older adults of T2DM patients attending Public Hospitals of Buno-Bedele Zone, Oromia region, Ethiopia, 2022.
Specific Objectives
Determining self-care practice among older adults of T2DM patients attending Public Hospitals of Buno-Bedele Zone, 2022.
Identifying factors associated with self-care practice among older adults of T2DM patients attending Public Hospitals of Buno-Bedele Zone, 2022.
Exploring the life experience of self-care practice among older adults of T2DM patients attending Public Hospitals of Buno-Bedele Zone, 2022.
Methods and Materials
Study Area and Period
This study was conducted in Buno-Bedele‘s four public Hospitals, in South West Ethiopia from April, 15/2022 to June, 20/2022. Buno- Bedele is located in western Oromia and is 480 kilometers far from Addis Ababa. Buno-Bedele has four hospitals and 32 health centers. In the hospital, there are different wards and clinics within the hospital the diabetic ambulatory clinic is one of the services provided.
Study Design
A facility-based mixed design was conducted to assess the self-care practice and associated factors of T2DM patients who had followed up at Buno Bedele four Public Hospitals.
Population
Source population
All T2DM patients with an age greater than 60 years and who had a follow-up at Buno-Bedele Public Hospitals were the source population.
Study Population
All selected T2DM patients with an age greater than 60 years, and who had follow-ups at Buno-Bedele Public Hospitals during the study period.
Inclusion and Exclusion Criteria
Inclusion Criteria
All selected T2DM patients with an age greater than 60 years and who had follow-ups for more than 6 months in Buno-Bedele Public Hospitals.
Exclusion Criteria
Patients (T2DM patients) who are unable to hear or communicate, and who are in serious clinical states were excluded from the study.
Sample size determination
The sample size is determined using a single population proportion formula. The proportion of type 2 DM self-care practice from the previous study (60.7%) at Nekemte Referral Hospital [22], was taken with the assumption of a 5% marginal error and 95% CI- The sample size was calculated as follows: n= (Zα/2)2 P (1-p) d2 Where n= number of the study subjects Z=the standardized normal distribution value for the 95% confidence interval (1.96) P = Type 2 DM self-care practice (60.7%) q=1-p =1-0.633 =0.393, p=0.607 and q =0.393 d = the margin of error taken as 5% = 0.05 n= (Zα/2)2 P (1-p) = (1.96)2 (0.607x0.393) = 367 d2 (0.05)2 By adding 10% (37) non-respondent rates the total sample size required for the quantitative study was 404.
For the qualitative study:
An in-depth interview was conducted to address the qualitative study part. Accordingly, 13 participants were selected purposively depending on the respondent‘s knowledge, diabetes long-term life experience, and motivation to participate.
Sampling Technique
For the quantitative part of the study: After calculating the sample size, four hospitals in Buno-Bedele were considered in the sampling process for the selection of the study subjects. The number of study participants from each 14 hospital was determined by proportion to population size by reviewing last year's report of older adults with T2 DM patients. The calculated sample size was distributed proportionally to each hospital based on their number of T2 DM reports. During the patient selection technique, the total T2DM population of each hospital was divided by sample size from hospitals we obtained the interval of two (2), then every two-interval patient was selected for interview. The first K (sampling interval) was determined for all hospitals by using lottery methods. Then, by using the systematic sampling method the data collectors interviewed the patient every two intervals on a daily basis at the time of follow-up from all hospitals until the required sample size allocated arrived. See figure 2 schematic presentation of the sampling procedure. The formula: ni = n/N * Ni Where n = total sample size to be selected N = total population Ni = total population of each hospital ni = sample size from each hospital
For the qualitative part of the study:
An in-depth interview was used to collect data. The T2DM patients from each hospital were purposely selected according to their willingness to participate.
Study Variables
Dependent variable: Self-care practice
Independent variables:
Socio-demographic characteristics (age, sex, residence, Income, Occupation, Educational status, marital status, Family support, and Social support) Diabetes-related clinical factors (FBS, type of DM medication, appointment adherence, DM complication, BMI (Body mass index), duration of DM, and having own glucometer)
Information-related factors (Television, Radio, Friends, Health care provider)
Individual Related Factors (Knowledge, and Attitude)
Operational definitions
Good self-care practice; Except for medication adherence (which required all 7 days), respondents were categorized as having "excellent self-care practice" if the total score was ≥ 60% of practice questions or variables under five components of self-care practice fell in the range of 4-7 days.) [18, 32].
Poor self-care practice; except for medication adherence (0-6 days), respondents were categorized as having "poor self-care" if the total score was < 60% of practice questions or variables under five components of self-care practice fell in the range of 0-3 days.) [18, 32].
Good knowledge: Patients with DM who score greater than or equal to the 50% of knowledge assessment questions [4].
Poor knowledge: Patients with DM who score less than 50% on knowledge assessment questions [4].
Diabetes self-care attitude:
Data was collected using statements on diabetic Self-care. Using the mean of a Likert scale of attitude measurement, patients were classed as having a favorable (above mean score) or unfavorable attitude (below mean score) toward diabetic self-care [4].
NB: Regarding computation for self-care practice status, five components (Physical activities, SMBG, medication adherence, foot care, and dietary selfcare practice) are needed. This method of computation and dichotomization was based on validated tool recommendations and previous related studies [17, 18].
BMI in Kg/M2 Underweight: < 18.50
Normal: 18.50 - 24.99
Overweight: 25 - 29.99
Obese: ≥ 30 based on recent updates [17].
Older age:- All person over age 60 years [3].
Data Collection Instrument
For the quantitative part of the study: The respondents were interviewed using structured questionnaires developed after a review of different kinds of literature used [18]. The questionnaire consisted of, 11 items of socio-demographic characteristics, 39 items of knowledge, 7 items for attitudes,16 items for practice (4 items dietary,2 items for physical activity, 2 items Self-monitoring of blood glucose, 3 items medication adherence 5 items foot care), and 2 items alcohol, and smoking assessment. The questionnaire contains five parts and 64 items for a quantitative study.
For the qualitative part of the study: The qualitative data were collected by using an open-ended semi-structured interview guided until the ideas of patients were saturated. The guide contains the benefit of self-care, challenges of self-care, the experience of their self-care practice, perception toward self-care, and best practice of self-care for DM. The voice recorded and notes were taken during an in-depth interview.
Data collection procedure
For the quantitative part of the study: The data was collected using a pretested structured face-to-face interview questionnaire prepared in English and translated into Afan Oromo. The data was collected by four BSc nurses from other institutions during follow-up. The interview was conducted in a separate area with protected privacy. And the data were collected after direct communication with the clients and reaching an agreement.
For the qualitative part of the study: The data were collected through face-toface, in-depth interviews. Face-to-face in-depth interviews were done using a semi-structured interview guide, prepared in English and translated into Afan Oromo. The investigator and supervisors conducted in-depth interviews. The data were collected through note-taking and tape-recording until the ideas of patients were saturated (an average of 40 minutes).
Data quality control
To assure the quality of tools properly aimed data collection tool was prepared and tested on 15% of the study sample (404), 60 participants at Agaro hospital were tested and entered into Cronbach‘s alpha by SPSS version 25 before the actual data collection period to assess the reliability.
Reliability statistics result from Cranach's Alpha=0.857 by using 16 Items of the diabetic self-care practice questionnaire. The data were collected using a well-structured interviewer-based questionnaire that is prepared in English and translated to Afan Oromo carefully trying to keep the consistency of the questions. Most questionnaires are prepared based on Ethiopian Diabetes Associations and Diabetes Education Program for People with Diabetes. The data collectors and supervisor were given brief one-day training concerning interviewing techniques and appropriate data recording. The collected data were checked for completeness, clarity, and consistency by the principal investigator. Furthermore; continuous coordination, monitoring, and supervision were carried out by the supervisor and principal investigator on a regular daily basis throughout data collection [18]. For the qualitative study part: Qualitative data were recorded by tape recorders and a note was taken for all comments to be understandable and useful, then clean-up of the transcripts by removing off not important words. I state thrust fullness and confidentiality was reserved for what I have taken information.
Data processing and analysis
Immediately after the data collection was completed, data were coded, edited, and entered into the computer software of Epidata version 4.6 and exported to SPSS Version 25 for analysis. Descriptive analysis was done to describe the number and percentages of the variables in the study. Tables and graphs were used to present the data. The bivariate logistic regression analysis was done to see the association between dependent and independent variables. P-values < 0.25 an association study variable was transferred to multiple logistic regression models. AOR with their 95 % confidence interval was computed, and a p-value < 0.05 was considered as the statistical significance in the multivariate model. Overall, model fitness was checked by Hosmer-Lemeshow goodness-of-fit. Multi-colinearity was checked by using variance inflation factors and the statistics result VIF=Range between 1.2 to 4.6 Qualitative data were recorded by tape recorders for all comments to be understandable and useful. The analysis was done using manually by grouping into themes. Different concepts and data categories were generated based on the objective of the study, and the information that was gained through the interview.
Ethical Consideration
As an important part of the study, the following step was taken to ensure the ethics of the study. The research and publication office of Salale University Health Science College approved this study. After approval by the University‘s research and publication office, each Hospital Administration has requested permission to proceed with the study. Before starting data, collection informed consent was taken from participating individuals, and the information was kept confidential for both qualitative and quantitative studies.
Results
Socio-demographic characteristics of the respondents
The data was collected from 386 patients with a 95.5% response rate. More than half 214 (55.4%) of the respondents were male, 241(62.4%) were in the age group of 61-70 years and 291 (75.4%) of participants were married. Three fourths 291 (75.4%) of participants belonged to the Oromo ethnic group. Furthermore, 94 (24.4%) had no formal education, and more than half 236 (61.1%) of the study participants have been living in urban areas. One hundred thirty-eight (35.8%) were farmers, and most of the respondents 291(75.4%) had family care and support (Table 1).
Table 1:- Socio-demographic Characteristics of T2DM Patients at Buno-Bedele Zone Public Hospitals, Oromia, Ethiopia, 2022 (n=386).
|
Variables |
Variables category |
Frequency |
Percent (%) |
|
Gender |
Male |
214 |
55.4 |
|
Female |
172 |
44.6 |
|
|
Age groups |
61-70 |
241 |
62.4 |
|
71-80 |
120 |
31.1 |
|
|
>=81 |
25 |
6.5 |
|
|
marital status |
Single |
28 |
7.3 |
|
Married |
291 |
75.4 |
|
|
Divorced |
24 |
6.2 |
|
|
Widowed |
32 |
8.3 |
|
|
Separated |
11 |
2.8 |
|
|
Occupation |
Farmer |
138 |
35.8 |
|
Merchant |
116 |
30.1 |
|
|
House wife |
48 |
12.4 |
|
|
Retired |
40 |
10.4 |
|
|
Others |
44 |
11.3 |
|
|
Ethnicity |
Oromo |
291 |
75.4 |
|
Amara |
65 |
16.8 |
|
|
Other |
30 |
7.8 |
|
|
Religion |
Protestant |
116 |
30.1 |
|
Orthodox |
98 |
25.4 |
|
|
Muslim |
150 |
38.9 |
|
|
Pagan |
22 |
5.7 |
|
|
Educational status |
Illiterate |
94 |
24.4 |
|
Grade 1-8 |
91 |
23.6 |
|
|
Grade 9-12 |
116 |
30.1 |
|
|
College and Above |
85 |
22 |
|
|
Place of residence |
Urban |
236 |
61.1 |
|
Rural |
150 |
38.9 |
|
|
Family history of DM |
Yes |
324 |
83.9 |
|
No |
62 |
16.1 |
|
|
Family care& support |
Yes |
262 |
67.9 |
|
No |
124 |
32.1 |
Diabetes-related clinical characteristics of the respondents
The majority 281 (72.8%) of respondents' duration of diabetes was greater than 20 years with a mean of 25.63±7.41, and 324 (83.9%) of them had a family history of diabetes, whereas significant numbers of 332(86%) respondents with BMI categorized as normal with mean 22.64±2.35. The mean of FBS for the last three visits was 191.85±56.50 and 49 (12.7%) of the respondents failed to adhere to appointments. About 364 (94.3%) had adherence on one or two medication. Regarding alcohol consumption and cigarette smoking, only 15(3.9%) of them drank alcohol, and 21 (5.4%) smoke a cigarette. The mean age during diagnosis of diabetes was 44.76±5.82 years, majority of 279 (72.3%) of the respondents had comorbidity, from comorbidity approximately half of 188 (48.7%) of them had hypertension and 107 (27.7%) had developed diabetes complication (Table 2).
Table 2: Diabetes-related clinical characteristics of the respondents at Buno Bedele Zone Public Hospitals, Oromia, Ethiopia, 2022 (n=386).
|
Variables |
Variables category |
Frequency |
Percent |
|
FBS 3 times Visit Category |
>130 mg/dl |
303 |
78.5 |
|
<130 mg/dl |
83 |
21.5 |
|
|
Duration of DM |
10-15 years |
38 |
9.9 |
|
|
16-20 years |
59 |
15.3 |
|
|
>20 years |
281 |
72.8 |
|
|
Others |
8 |
2.0 |
|
BMI category |
18.5-24.9 |
332 |
86.0 |
|
|
25-29.9 |
39 |
10.1 |
|
|
>30 |
11 |
2.8 |
|
Others |
4 |
1 |
|
|
Follow up adherence |
Yes |
337 |
87.3 |
|
|
No |
49 |
12.7 |
|
Type Of Medication |
OHA |
204 |
52.8 |
|
|
Insulin |
115 |
29.8 |
|
|
OHA and Insulin |
67 |
17.4 |
|
Medication adherence |
Yes |
364 |
94.3 |
|
|
No |
22 |
5.7 |
|
DM Complication |
Yes |
109 |
28,2 |
|
|
No |
277 |
71.8 |
|
Family history of DM |
Yes |
324 |
83.9 |
|
|
No |
62 |
16.1 |
|
Presence of co-morbidity |
Yes |
279 |
72.8 |
|
|
No |
107 |
27.2 |
|
Type of co-morbidity |
HPN |
188 |
48.7 |
|
|
Heart Failure |
54 |
14.0 |
|
|
kidney disease |
22 |
5.7 |
|
|
No co-morbidity |
107 |
27.7 |
|
|
Others |
15 |
3.9 |
|
Presence of own glucometer |
Yes |
16 |
4.1 |
|
|
No |
370 |
95.9 |
NB:-Others for duration of DM <10 years Others for BMI <18.5
Others type of comorbidity:-Dermatitis and peptic ulcer disease
Information-related diabetes self-care practice
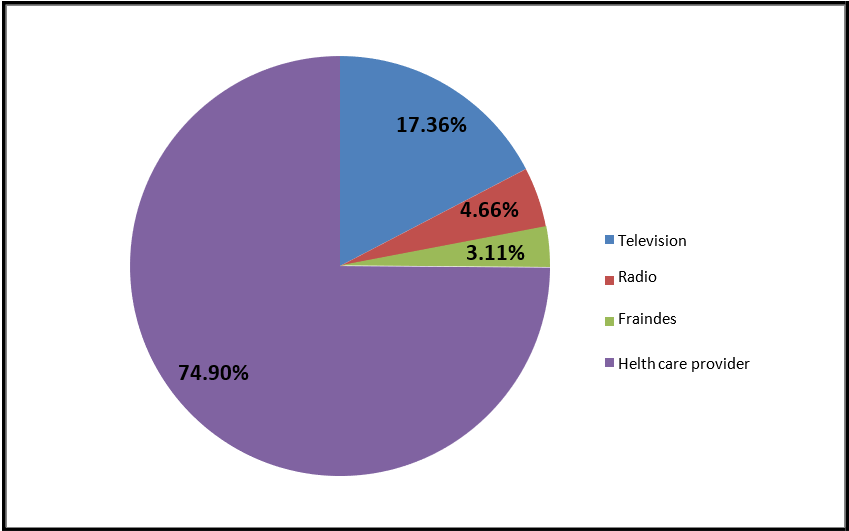
Regarding information related to diabetes self-care practice majority of 289 (74.9%) of the respondents get information from health care providers, 67 (17.4%), 18 (4.7%), and 12 (3.1%) got information from television, radio, and friends respectively. Figure 1 illustrates information related to T2DM self-care practice.
Figure 1: Information-related diabetes self-care practice of T2DM Patient at Buno-Bedele Zone Public Hospitals, Oromia, Ethiopia, 2022 (n=386).
Knowledge Regarding Diabetes self-care practice
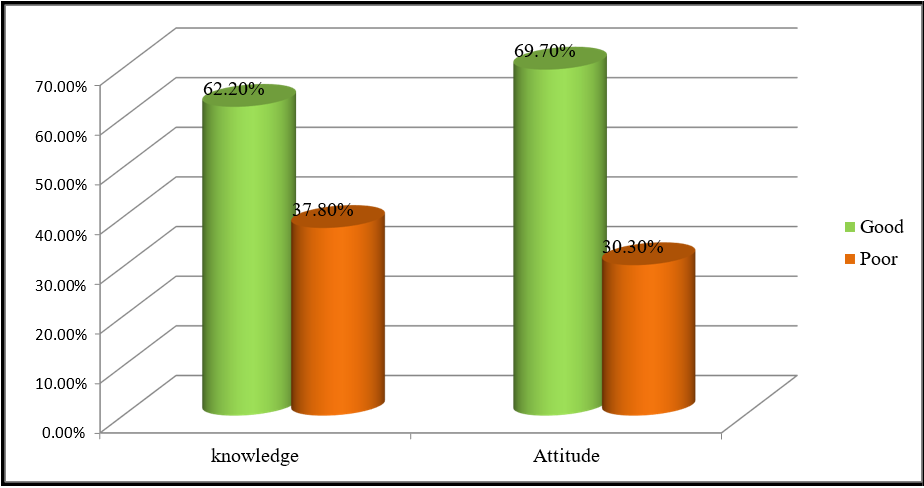
The evaluation of knowledge showed that the majority of 240 (62.2%) of the study participants had high overall knowledge about diabetic self-care practice while the rest (37.8%) had low knowledge of diabetic self-care practice (Figure 4). The mean (±SD) of knowledge score for the study participants was found to be 10.80 ±2.88 with a maximum and minimum possible score of 19 and 5 respectively. Of the majority of participants, 288(74.6%) knew self-management of hypoglycemia. However, only 135 (35%) participants had knowledge of acute (short-term) and long-term DM complications. Of most of the participants, 326(84.5%) had good knowledge of the signs and symptoms of hyperglycemia, while 355(92%) participants had good knowledge about hyperglycemia management. Regarding hypoglycemia 329(85.2%) participants had awareness of the signs & symptoms of hypoglycemia, while 283(73.3%) participants had good knowledge and management of hypoglycemia (Table 3).
Table 3:- Diabetes-related clinical characteristics of the respondents at BunoBedele Zone Public Hospitals, Oromia, Ethiopia, 2022 (n=386).
|
Knowledge toward DSCP |
Participant Response |
Frequency |
|||
|
Yes |
No |
||||
|
N |
% |
N |
% |
||
|
DM definition |
Knowledge of DM definition |
122 |
31.6 |
264 |
68.4 |
|
Hyperglycemia |
Knowledge of signs and symptoms of hyperglycemia. |
326 |
84.5 |
60 |
15.5 |
|
Hyperglycemia |
Knowledge of hyperglycemia management |
355 |
91.9 |
31 |
8.1 |
|
Hypoglycemia |
Knowledge of signs and symptoms of hypoglycemia. |
329 |
85.2 |
57 |
14.8 |
|
Hypoglycemia |
Knowledge of hypoglycemia management |
283 |
73.3 |
103 |
26.7 |
|
DM complication |
Knowledge of short-term and long-term diabetic complication |
135 |
35 |
251 |
65 |
Attitude Status toward Diabetic Self-care practice
Attitude status toward diabetic self-care practice: The overall prevalence of favorable attitude toward T2DM was 69.7% while the unfavorable attitude was 30.3% (Figure 4). The mean ±SD of attitude score for the study participants was found to be 3.085±0.820. The majority of the study participants 269 (69.7%) had a favorable attitude score greater than the mean, indicating they had a positive attitude toward diabetes self-care practice. More than half 222 (57.5%) of the respondents reported that controlling the food to be taken is believed effective way of diabetic management, and 210 (54.4%)regular exercise like walking for 30 min/day, 3-5 days a week improves the health of diabetic patients. Furthermore, 213(55.2%) of the participants reported that the health education given to diabetic patients during follow-up visits is very important (Table 4).
Figure 2:- The overall prevalence of knowledge and attitudes towards T2DM Patient at Buno-Bedele Zone Public Hospitals, Oromia, Ethiopia, 2022 (n=386).
Table 4: Attitude towards Self-care Practice among T2DM Patients on Followup at Buno-Bedele Zone Public Hospitals, Oromia, Ethiopia, 2022 (n=386).
|
Attitudes towards DSCP |
Number of study participants (percentage) |
||||
|
Strongly disagree |
Disagree |
Neutral |
Agree |
Strongly agree |
|
|
Weight loss can prevent the complications of DM. thus, it is important to lose weight |
164(42.5%) |
175(45.3%) |
9(2.3%) |
29(75%) |
9(2.3%) |
|
Making the necessary lifestyle changes for DM is very mandatory |
34 (8.8%) |
176 (45.6%) |
21(5.4%) |
70(18.1%) |
85(22.0%) |
|
Follow-up is needed for all patients? |
77 (19.9%) |
124(32.1%) |
21(5.4%) |
106(27.5%) |
58(15.0%) |
|
Controlling the foods to be taken is an effective way of managing DM. |
12 (3.1%) |
125(32.4%) |
27(7.0%) |
126(32.6%) |
96(24.9%) |
|
The diabetic education given at follow-up visits is important |
13 (3.3%) |
128(33.2%) |
32(8.3%) |
101(26.2%) |
112(29.0%) |
|
Walking 30min/day 5 days a week improves the health of DM patients |
19 (49%) |
129(33.4) |
28(7.3%) |
81(21.0%) |
129(33.4%) |
|
All diabetic patients should stop smoking |
22 (5.7%) |
118(30.6) |
21(5.4%) |
64(16.6%) |
156(40.4%) |
Self-care Practice toward Diabetes
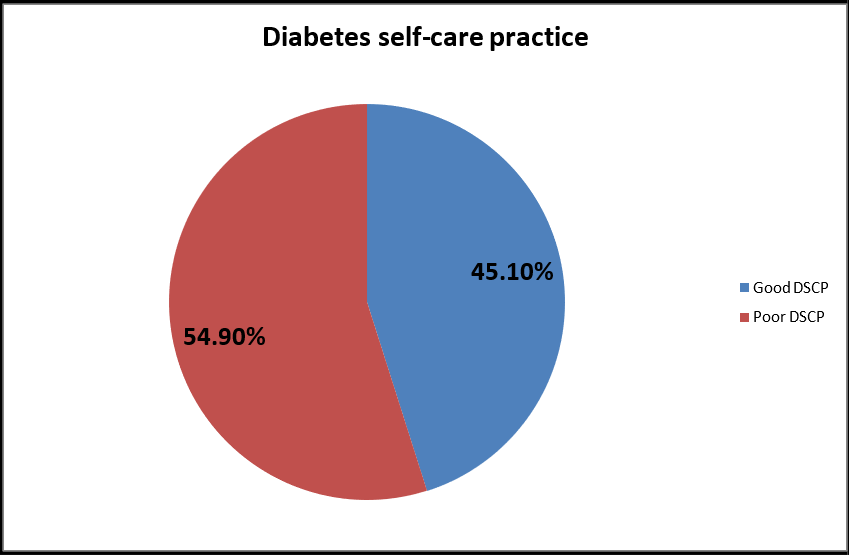
The overall prevalence of good DSCP was 45.1% whereas 54.9% of participants were poor practices (Figure 5). The mean ±SD of the self-care practice score for the participants was 4.69±1.133 (range: 5.27; minimum 1.64 Max 6.90). One hundred seventy-four (45.19%) of the study participants had good self-care practice. Self-care practices that were best followed were adherence to no smoking, 365 (94.6%), adherence to medication, 364(94.3%), and adherence to no alcohol intake 371 (96.1%). Out, 63(16.3%) participants had their own glucometer at home, and 54 (14%) adherence for testing of their blood glucose. Regarding physical activities, 163(42 %) of them advised exercising continuously for 30 minutes at least 3 days per week, 201(52%) participants had adherence to a healthy diet plan, and the majority of the participants, 319(82.6%) had good foot care practice (Table 5).
Figure 3:- The overall self-care practice of T2DM Patient at Buno-Bedele Zone Public Hospitals, Oromia, Ethiopia, 2022 (n=386).
Table 5:- Frequency Distribution of Self-care Practice among T2DM Patients on Follow-up at Buno-Bedele Zone Public Hospitals, Oromia, Ethiopia, 2022 (n=386).
|
DSCP Assessment |
Participant Response |
Frequency |
|||
|
Yes |
No |
||||
|
N |
% |
N |
% |
||
|
Diet |
Healthful eating plan in the last 7days |
136 |
35.2 |
250 |
64.8 |
|
Eat five or more servings of fruits and vegetables in the last 7days |
294 |
76.2 |
92 |
23.8 |
|
|
Did you space carbohydrates evenly through the day In the last 7 days? |
174 |
45.1 |
212 |
54.9 |
|
|
Average diet practice in the last 7 days |
201 |
52 |
185 |
48 |
|
|
Physical Activity |
Did you participate in at least 30 minutes of physical activity In the last 7days? |
164 |
42.5 |
222 |
57.5 |
|
Did you participate in a specific exercise session in the last 7 days? |
161 |
41.7 |
225 |
58.3 |
|
|
Average physical activity in the last 7 days |
163 |
42 |
223 |
58 |
|
|
Self-monitoring of blood glucose |
Did you test your blood sugar the number of times recommended by your health care provider? |
11 |
2.8 |
375 |
97.2 |
|
Foot care |
Did you check your feet in the last 7days? |
321 |
83.2 |
65 |
16.8 |
|
Did you inspect the inside of your shoes every day? |
322 |
83.4 |
64 |
16.6 |
|
|
Did you wash your feet every day? |
314 |
81.3 |
72 |
18.7 |
|
|
Did you dry between your toes after washing? |
319 |
82.6 |
67 |
17.4 |
|
|
Total foot care in the last 7days |
319 |
82.6 |
67 |
17.4 |
|
|
Medication adherence |
Did you take your recommended DM medication? |
364 |
94.3 |
22 |
5.7 |
Factors associated with overall diabetes self-care practice
Bivariate logistic regression analysis workup rated seven variables (Type of DM medication, age group, diabetes complication, family care & support, have own glucometer, attitude, and appointment adherence) as candidates for multivariable logistic regression by the filtering standard P value < 0.25. Whereas in multivariable logistic regression analysis output assured five variables (diabetes complication, appointment adherence, have own glucometer, family car & support, and attitudes) were predictors of overall self-care practice by minima of P value <0.05 (Table 7). Results from binary logistic regression showed that the odds of participants who had good perception (attitudes) were 2.03 times more positive attitudes towards diabetic self-care practice than those who had unfavourable attitudes [(AOR=2.03; 95% CI: (1.13–3.64)]. Participants who had family care and support were 3.01 times more likely to perform DM self-care practice than those who had no family care & support [(AOR=3.01; 95% CI: (1.680-5.412). Participants who had DM complications were 6.56 times more likely to practice self-care when compared to those who had no complications [(AOR=6.56; 95% CI: (3.375-12.765)]. Participants who had their own glucometer were 5.78 times do diabetic self-care practice when compared to those who had no own glucometer [(AOR=5.78; 95% CI: (2.14-12.52)]. The patient who had follow-up adherence was 3.84 times more likely to do DSCP when compared to the contrast [(AOR=3.84; 95% CI: (1.680- 5.412)] (Table 6).
Table 6: Factors associated with diabetes self-care practice of patients on follow up at Buno-Bedele public Hospitals, Oromia, Southwest Ethiopia, 2022 (n=386).
|
Variables |
Self-care practice |
Crude Odds Ratio with 95% CI |
P-value |
Adjusted Odds Ratio with 95% CI |
P-value |
|
|
Good |
Poor |
|||||
|
Age groups |
|
|
|
|
|
|
|
61-70 |
131 |
110 |
4.76(1.73-13.11) |
0.001 |
1.40(0.80-2.94) |
0.242 |
|
71-80 |
38 |
82 |
1.85(1.73-13.11) |
0.003 |
1.05(0.60-5.65) |
0.283 |
|
> =81 |
5 |
20 |
1 |
|
1 |
|
|
Family support |
|
|
|
|
|
|
|
Yes |
150 |
112 |
5.58(3.36-9.28) |
0.001 |
3.01(1.68-5.41) |
0.001** |
|
No |
24 |
100 |
1 |
|
1 |
|
|
Good appointment |
|
|
|
|
|
|
|
Yes |
166 |
171 |
4.98(2.27-10.93) |
0.001 |
3.84(1.60-9.19) |
0.003** |
|
No |
8 |
41 |
1 |
|
1 |
|
|
Attitude of DSCP |
|
|
|
|
|
|
|
Favorable ADSCP |
150 |
119 |
4.88(2.94-8.13) |
0.001 |
2.03((1.13-3.64) |
0.019* |
|
Unfavorable |
24 |
93 |
1 |
|
1 |
|
|
DM Complication |
|
|
|
|
|
|
|
Yes |
93 |
16 |
14.07(7.79-25.38) |
0.001 |
6.56(3.38-12.77) |
.001** |
|
No |
81 |
196 |
1 |
|
1 |
|
|
Have glucometer |
|
|
|
|
|
|
|
Yes |
54 |
9 |
10.15(4.84-21.29) |
0.001 |
5.20(2.14-12.52) |
.001** |
|
No |
120 |
203 |
1 |
|
1 |
|
Qualitative Study Findings
A total of 13 in-depth interviews were conducted with T2DM patients. Eight of the participants were males, and the participants‘ age ranged from 61 to 80 years. All of the participants reported positive family history of T2DM. Regarding the educational status of the participants, two of them were MA qualified degrees, four patients have a BSc degree, two have a diploma, three patients were secondary school graduates and two respondents have no formal education. Four participants were using insulin medication alone, five were using oral antidiabetics, and four were using insulin plus metformin. From key informants' data obtained, five themes emerged. These are knowledge of DM, good adherence to medication and medical advice, challenges of diabetes self-care practice, self-care benefits, and recognition of diabetes complications.
Knowledge of diabetes
Informants described the recognition of DM as having high blood sugar levels, understood diabetes hypoglycemia, and a chronic condition that requires enduring care for the remainder of their lives. However, a few informants thought of diabetes as fluctuating blood glucose levels similar to mental illness mood changes. A 65-year-old man informant narrated: "Simply diabetes mellitus is an elevation in blood glucose level." A 61-year-old male informant stated that diabetes is permanent living with individuals that are not curable. He said: "Diabetes is an incurable disease we will live together until death." A 75-year-old male informant described diabetes as increasing RBS with mood changes like mental illness. The fluctuation of blood sugar is related to stress and mood change. "Diabetes is an increment of blood glucose level that varies with unpredictable mood like a mental disorder." A 65-year-old male and 67-year-old female key informant described the knowledge of hypoglycemia symptoms during their repeated experience of this hypoglycemia. They stated that:
Hypoglycemia is characterized by a low level of blood glucose that I recognized by its sign; palpitation, sweating, and dizziness.
Good adherence to medication and medical advice
Key informants described that adhering to medication and health care provider advice is crucial to have controlled blood sugar. The informants mentioned that using health care advice and timetable as well as regular follow-up is beneficial to keep the diabetes mellitus normal. A 72-year-old male informant explained that good adherence to medication is beneficial to control blood sugar. He said that: "My blood glucose level increased if I am too late to take my insulin. As I think if I take medication appropriately on time it is good for controlling blood sugar." A 67-year-old man narrated that taking medication on time and when missing can cause high blood sugar. He described as below:
"If I forget to take a medication, my blood glucose level rises. Keeping doctors’ advice and taking medication on time is the most important as I observed on myself."
Challenges of diabetes self-care practice
Most of the key informants described that the most challenging to control diabetes mellitus are advanced age, forgetfulness to take medication, low socioeconomic status, poor family support, and shortage of medication supply, particularly those informants who take insulin were at risk of time-to-time shortage happened. 65 years old female said that she had poor family care and support and she was dependent so, she couldn‘t keep a healthy eating plan, she didn‘t go follow-up regularly, she didn‘t take medication continuously and she said ―she was suffering from signs of hypoglycemia, and hyperglycemia frequently‖. 77-years old male narrated ―I‘m living alone I didn‘t go follow-up regularly" Regular follow-up is very important unless I kept appointments, I didn‘t know my blood glucose status and I didn‘t get medication. An 80-year-old male key informant said that even minimum activities are important for controlling blood sugar. He described as:
"When I consumed honey and did not work out any physical activities my blood sugar level was increased. Even though I am aged to do heavy activities I am only walking in my house." A 65-year-old male key informant described the shortage of insulin in their hospital and experienced high blood sugar several times. He stated;
"The big challenge is insufficient insulin I have experienced twice a shortage of insulin and they referred me to another hospital, which cost me more money. " Similarly, a 68-year-old female informant said that:
"I do have not enough money; I am supported by my family for buying this medication. Nevertheless, if it is found in this hospital I take it free without costing anything. However, sometimes did not obtain from the hospital."
Self-care benefit
It is obvious that self-care is important to control blood sugar. Most of the key informants told out that consuming fatty food and sweet drinking are increasing the level of sugar. However, self-care practices including physical exercise, daily foot care, medication adherence, controlling sweet drinks, foods, and self -monitoring blood sugar are made effective for diabetes mellitus control. The majority of key informants reported that having good family care and social support increases their health in controlling their glucose levels. A 69-year-old female said that: ‖If you had a glucometer at home it is an easy way of monitoring self-blood glucose monitoring and having your own glucometer for DM patients is mandatory to keep self-blood glucose monitoring‖. "If I consume a lot of fatty food and sweets drinker, my blood sugar increases. So self-care is very important to control diabetes with regular control of blood sugar, avoiding sweet drink, and high fatty contains food." Additionally, a 70-year-old female key informant described the benefit of self-care practice as follows: "When my blood glucose level is high, I usually reduce the size of my meal and stop eating sweets for a few days. I check my blood sugar level and regularly I take my medication with the advice of a health care provider‘s." A 68-year-old woman stated that "avoiding consumption of fatty food and drinks are best self-care practice."
Recognizing Diabetes Complications
The key informants described the complications related to diabetes mellitus including heart disease; stroke, vision issues, neuropathy, renal failure, erectile dysfunction, and diabetic foot ulcer were among the complications that were reported. A 61-year-old male informant mentioned that loss of vision is the most frequent and worst complication of diabetes mellitus. He mentioned that renal and heart diseases are the additional worst complication. He said that: According to my understanding, the worst complication of diabetes is losing vision. In addition, renal failure and heart disease is also the worst thing. On the other hand, an 80-year-old male informant stated that stroke is the worst complication that he suffered from the complication of diabetes mellitus. He narrated as below:
"Stroke is the worst complication, look at me, I can’t walk steadily and my mouth is skewed. “A 69-year-old female informant explained that as blood sugar increases, there is an increase in the amount of urine output and dry lip and mouth. She stated as below:
"When my blood glucose is above normal, I feel dry lips and mouth, then an increase in the amount of urine." A 73-year-old male informant explained that diabetes can affect all organs and is compared to cancer. He stated that: "Because diabetes can harm every organ in the body, diabetes is comparable to cancer."
Discussion
The present study was done to assess diabetes self-care practice among patients attending at Buno-Bedele public hospitals. In this study, 45.1% (95% of CI: 39.9- 49.7) of patients had good diabetes self-care practices. This study was consistent with the study done in Tigray regional public hospitals (46.7%) [38] and a study conducted at Hawassa University, College of Medicine (47.8%) [23]. This finding was lower than the study done in Harar and Dire Dawa hospital (64.4%)(Ayele and Mengesha, 2019) Nekemte Referral Hospital(60.7) [22], Jimma university (54.2%) (28), in Benishangul Gumuz Regional State Public Hospital (54.3%) [12], in India (76.9%) [28] and in Gondar University of College of Medicine and Health (54.04%) [37]. This finding was higher than the study done in Bahir Dar, Northwest Ethiopia (28.4%) [14] and study done in the central zone of Tigray public Hospitals (37.3%) [11]. This study is done among older adults above age 60 and additionally, this might be due to the different settings used by the other study. The availability of a personal glucometer at home was significantly associated with good diabetes self-care practice, This finding is also supported by other studies conducted in Tigray public hospitals (38), in the central zone of Tigray, Ethiopia [11], and in Nekemte Referral Hospital [22]. However, the availability of a personal glucometer was very low (16.3%) in this study.
Similarly, a study done in Tigray public hospitals (11.9%) [38] and a systematic review of sub-Saharan countries revealed on average only 15% of all patients were able to test their blood glucose levels at home [33]. A 69-year-old female said that: If you had your own glucometer at home it is an easy way of monitoring sel fblood glucose monitoring and having your own glucometer for DM patients is mandatory to keep self-blood glucose monitoring. The outcome variable of good self-care practices was significantly associated with those who had positive attitudes toward diabetes self-care practice when compared to their counterparts. This study was in line with the study in Nigeria [25] which found that good self-care practices were more prevalent. It is true that having positive expectations of advantages is frequently identified as a crucial component in engaging in a particular health self-care practice activity. This study contradicts with research conducted in Harare Town [20], and it is 70% less likely to be related to the outcome variable. This might be because of a lack of commitment to self-care practices brought on by a negative attitude about the illness and the general level of education of the propulsions. Patients who had strong family support had self-care practice as compared to patients who had no family support. This study was supported by different studies [21, 34]. The possible reasons could be social support from family or friends as a form of psychological support, informational and financial can help the patient to cope with problems and give strength in self-care practice. A systematic review of 23 series of studies related to the impact of DSCP involving family care and support as a fundamental source of social support on self- care practice among T2DM patients between 2008 and 2016 confirmed the impact of family care and support integration on several health outcomes of T2DM [34]. 65 years old female said that “she had poor family care and support and she was dependent so, she couldn’t keep a healthy eating plan, she didn’t go follow-up regularly, she didn’t take medication continuously and she was suffering from signs of hypoglycemia, and hyperglycemia frequently”.
Patients with diabetic complications managed their illness better by seeking help from their families and were more likely to practices and adopt Good diabetes self-care practice compared to those without any complications in this study. This study revealed that they adhered more to the instructions given by their physician. On the opposite, patients who have no complications may not worry much to adhere to self-care practices. This study association between DM complications and self-care practice is in line findings reported in Harar and Dire Dawa: A hospital study [20]. Patients who had good follow-up adherence were 3.84 [AOR=3.84; 95% CI: (1.60-9.19)] times more likely to do DSCP when compared to the opposite. This study is in line with the study conducted in Southern Dawuro Tarecha Hospital, which indicates respondents who had good adherence to appointment six times more apply self-care practice than those who didn‘t follow up on their appointments [18]. Another study indicated that patients who frequently miss appointments are more likely to struggle with other facets of self-care practice. Fortunately, in most clinical contexts, adherence to appointment-keeping can be evaluated very easily [30]. 77-years old male narrated “I’m living alone I didn’t go follow-up regularly" Regular follow-up is very important unless I kept appointments, I didn’t know my blood glucose status and I didn’t get medication”.
Conclusion
Overall, older adult patients with Type 2 diabetes in Buno-Bedele Public Hospitals exhibit low diabetes self-care practices. Diabetes self-care practices are significantly associated with family care & support, diabetes complication, favourable attitudes, having your own glucometer, and appointment adherence was significantly associated with good diabetes self-care practice. While knowledge of diabetes self-care practice had a positive impact on diabetes selfcare practices of Type 2 older diabetic patients in this study, and the majority of the quantitative study findings were supported by the qualitative approach.
Strength
This study utilized both quantitative and qualitative methods approach to identify factors associated with self-care practice, incorporating elderly adults only. Self-care practice of study participants was supported by a mixed method study.
Limitation
Limitation of related literature in Ethiopia to compare and contrast the finding officially with the studies conducted in the country. The nature of the cross sectional study design had not better identify factors affecting self-care practice in real parameter. The results of mixed methods are difficult to integrate.
Recommendation
For policy/decision makers (PMO, MOH, DM SOCIETY, & NGOs) According to a study, there is a need to build policies and programs that are intended to change how people practice self-care and their level of glycemic control or to create training guidelines and curricula that are supported by visual aids. The implementers should therefore accept that diabetes self-care practices are important public health issues and accord to altering policies.
For Health professions It‘s better if functional multidisciplinary teams are composed of doctors, nurses, dieticians and diabetes educators. Has to be organized, and routinely assess selfcare practice and monitor how diabetes patients are going to control their blood glucose. It is very important to take into consideration the following facts to improve the situation of diabetic patients: Regional Health Bureau and Zonal Health Department in coordination with Buno- Bedele Public hospitals (Bedele Hospital, Didessa Hospital, Chawaka Hospital, and Chora Hospital) and the Diabetic Association Coordinators should have to develop health information dissemination programs and strategies that consider the low diabetes self-care practice, especially in older adults status, to reduce complications, to enhance the perception of the patient with diabetes self-care practice, to improve the awareness family members of diabetic patients about diabetes self-care and the importance of self-care practices. Buno-Bedele Hospital Administers and Diabetic Association Coordinators should reinforce the diabetic patients on follow-up and health professionals working in the diabetic clinic to improve their knowledge of diabetes and its self-care. Furthermore it‘s better if maximal effort has to be used to break the cycle of low income to resolve the deficit of materials necessary for self-care practice and in turn glycemic control such as glucometers, availability of medication. E.g., working with NGO and attempting free services like HIV /AIDS, or full filling vital instruments such as glucometers for seriously poorest societies. Prepare routine health information dissemination and should be given by trained and experienced health professionals by considering the patient's educational background, occupation, age, and years of suffering from the disease. All nurses‘ workings on diabetes should give strict advice on the importance of self-care practices for diabetic patients during their follow-up schedule and develop educational programs and activities to educate patients on the prevention and treatment of diabetes and should not rely on medical intervention only.
For researcher’s The researcher‘s, further study should look into the sustainability of the self-care practice among older adults to reduce diabetic-related morbidity and mortality. It‘s better for the researcher to conduct further studies, since there is a need for doing increasingly researches at the national level and there was no/ limited study conducted among older diabetic patients specially in Ethiopia on diabetes self-care practice.
Acknowledgement
We would also like to express my gratitude to Salale University College of Medical and Health Sciences for allowing us to undertake this research thesis. Also, we would like to thank the staff of chronic diabetes mellitus follow-up at Buno Bedele Zone public Hospitals, the study participants as well as data collectors for their time and unreserved cooperation.
Conflict of Interest: Author declares no conflict of interest
Funding: Not available
References
- Ogurtsova K, da Rocha Fernandes JD, Huang Y, Linnenkamp U, Guariguata L, et al. (2017) ‗IDF Diabetes Atlas : Global estimates for the prevalence of diabetes for 2015 and 2040. Diabetes Research and Clinical Practice. 128: 40–50.
- International Diabetes Federation (IDF). IDF Diabetes (2022) International Diabetes Federation (IDF). IDF Diabetes ,2022-08- 14, IDF. (Accessed: 14 August 2022).
- Werfalli M.M, Kalula SZ, Manning K, Levitt NS (2020) Does social support effect knowledge and diabetes self-management practices in older persons with Type 2 diabetes attending primary care clinics in Cape Town, South Africa?. PLoS ONE. 15(3):.
- Chen L, Magliano D.J, Zimmet P.Z (2012) The worldwide epidemiology of type 2 diabetes mellitus - Present and future perspectives. Nature Reviews Endocrinology. 8(4): 228–236.
- Kart C.S (2011) NIH Public Access. 23(4): 361 –376.
- Mier N, Medina A.A, Ory M.G (2007) Mexican Americans with type 2 diabetes: Perspectives on definitions, motivators, and programs of physical activity. Preventing Chronic Disease. 4(2): A24.
- Molalign Takele G, Weharei MA, Kidanu HT, Gebrekidan KG, Gebregiorgis BG (2021) Diabetes self-care practice and associated factors among type 2 diabetic patients in public hospitals of Tigray regional state, Ethiopia : A multicenter study. PLoS One. 16(4): e0250462.
- Aschalew AY, Yitayal M, Minyihun A, Bisetegn TA (2019) Self-care practice and associated factors among patients with diabetes mellitus on follow up at University of Gondar Referral Hospital. BMC Research Notes. 12(1): 591.
- Davies MJ, D'Alessio DA, Fradkin J, Kernan WN, Mathieu C, et al. (2018) Management of hyperglycemia in type 2 diabetes, 2018. A consensus report by the American Diabetes Association (ADA) and the european association for the study of diabetes (EASD). Diabetes Care. 41(12): 2669–2701.
- Ahmad Sharoni SK, Abdul Rahman H, Minhat HS, Shariff- Ghazali S, Azman Ong MH (2018) The effects of self-efficacy enhancing program on foot self-care behaviour of older adults with diabetes: A randomised controlled trial in elderly care facility, Peninsular Malaysia. PLoS ONE. 13(3): e0192417.
- Whiting DR, Guariguata L, Weil C, Shaw J (2011) IDF Diabetes Atlas: Global estimates of the prevalence of diabetes for 2011 and 2030‘, Diabetes Research and Clinical Practice. 94(3): 311 –321.
- Mariye T, Tasew H, Teklay G, Gerensea H, Daba W (2018a) Magnitude of diabetes self-care practice and associated factors among type two adult diabetic patients following at public Hospitals in central zone, Tigray Region, Ethiopia, 2017. BMC Research Notes. 11(1): 380.
- Chali S.W, Salih M.H, Abate A.T (2018a) Self-care practice and associated factors among Diabetes Mellitus patients on follow up in Benishangul Gumuz Regional State Public Hospitals, Western Ethiopia: A cross-sectional study. BMC Research Notes. 11(1): 833.
- Powers MA, Bardsley JK, Cypress M, Funnell MM, Harms D, et al. (2020) Diabetes Self-management Education and Support in Adults With Type 2 Diabetes: A Consensus Report of the American Diabetes Association, the Association of Diabetes Care & Education Specialists, the Academy of Nutrition and Dietetics, the American Academy. Diabetes Educator. 46(4): 350–369.
- Abate TW, Tareke M, Tirfie M (2018a) Self-care practices and associated factors among diabetes patients attending the outpatient department in Bahir Dar, Northwest Ethiopia. BMC Research Notes. 11(1): 800.
- American Diabetes Association (2020a) Facilitating Behavior Change and Well-being to Improve Health Outcomes : Standards of Medical Care in Diabetes d 2020‘, 43(Supplement_1): 48–65.
- American Diabetes Association (2016) Standards of Medical Care in Diabetes— 2016 Abridged for Primary Care Providers. Clinical Diabetes. 34(1): 3–21.
- Rasoda Saumika MA, Amarasekara T, Jayasekara R (2019) Diabetes Self-Care Activities and Glycaemic Control among Adults with Type 2 Diabetes in Sri Lanka : A Cross-Sectional Study. 7(5): 99–111.
- Ataro, B.A. and Argaw, Z. (2020) Pr ep rin t n ot er r Pr t n ot pe er ed‘, 1.
- Ayele BH, Mengesha MM, Tesfa T (2019) Predictors of self-care activities of outpatient diabetic residents in Harar and Dire Dawa : A hospital-based cross-sectional study. SAGE Open Med. 7: 2050312119865646.
- Ayele K, Tesfa B, Abebe L, Tilahun T, Girma E (2012) Self Care Behavior among Patients with Diabetes in Harari , Eastern Ethiopia : The Health Belief Model Perspective Self Care Behavior among Patients with Diabetes in Harari , Eastern Ethiopia: The Health Belief Model Perspective. PLoS One. 7(4): e35515.
- Dalgard O.S, Dowrick C, Lehtinen V, Vazquez-Barquero JL, Casey P, et al. (2006) Negative life events, social support and gender difference in depression. Social Psychiatry and Psychiatric Epidemiology. 41(6): 444–451.
- Dedefo MG, Ejeta BM, Wakjira GB, Mekonen GF, Labata BG (2019) Self-care practices regarding diabetes among diabetic patients in West Ethiopia. BMC Research Notes. 12(1): 212.
- Degefa G, Wubshet K, Tesfaye S, Hirigo AT (2020) Predictors of Adherence Toward Specific Domains of Diabetic Self-Care Among Type-2 Diabetes Patients. Clinical Medicine Insights: Endocrinology and Diabetes. 13: 1179551420981909.
- Ishak NH, Mohd Yusoff SS, Rahman RA, Kadir AA (2017) Diabetes self-care and its associated factors among elderly diabetes in primary care. Journal of Taibah University Medical Sciences. 12(6): 504–511.
- Jackson IL, Adibe MO, Okonta MJ, Ukwe CV (2014) Knowledge of self-care among type 2 diabetes patients in two states of Nigeria. Pharmacy Practice. 12(3): 404.
- Mekonnen Y, Hussien N (2021) Self-care related knowledge, attitude, and practice and associated factors among patients with type 2 diabetes in JMC, Ethiopia. Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy. 14: 535–546.
- Uma Maheshwari R, Sowmiya K.R, Kavin S (2017) Self-care practices among type II diabetics attending primary health centre, Thiruvallur district, Tamil Nadu‘, International Journal Of Community Medicine And Public Health. 4(8): 2745.
- Robinson D.N (1968) Visual disinhibition with binocular and interocular presentations. Journal of the Optical Society of America. 58(2): 254–257.
- Sisay Gedamu A, Sewunet Ademe K, Samuel Anteneh A, Abebe Dires N, Kirubel Dagnaw T (2021) Self-care practice and associated factors among type 2 adult diabetic patients on follow up clinic of Dessie referral hospital, Northeast Ethiopia. Clinical Journal of Nursing Care and Practice. 5(1): 031–037.
- Stephani V, Opoku D, Beran D (2018) Self-management of diabetes in Sub-Saharan Africa : a systematic review. BMC Public Health. 8(1): 1148.
- Glasgow RE, Toobert DJ (1988) Social Environment and Regimen Adherence Among Type II Diabetic Patients. Diabetes Care. 11(5): 377-86.
- Tuha A, Getie Faris A, Andualem A, Ahmed Mohammed S (2021) Knowledge and practice on diabetic foot self-care and associated factors among diabetic patients at dessie referral hospital, northeast ethiopia: Mixed method. Diabetes, Metabolic Syndrome and Obesity. 14: 1203–1214.
- Wolf MS, Davis TC, Curtis LM, Bailey SC, Knox JP, et al. (2016) A Patient-Centered Prescription Drug Label to Promote Appropriate Medication Use and Adherence. Journal of General Internal Medicine. 31(12): 1482–1489.
- Yehualashet F.A, Takele WW, Tegegne ET, Ayele AD (2019) Diabetics ‘ self-care practice and its determinants among Adult diabetic patients in Ethiopia : A systematic review and meta- analysis . Diabetics ‘ self- care practice and its determinants among Adult diabetic patients in Ethiopia : A systematic review‘.
- Molalign Takele G, Weharei MA, Kidanu HT, Gebrekidan KG, Gebregiorgis BG (2021) Diabetes self-care practice and associated factors among type 2 diabetic patients in public hospitals of Tigray regional state, Ethiopia: A multicenter study. PLoS One. 16(4): e0250462.