Mariana Santos1*, Sofia Almeida Xavier1, Margarida Lopes2, Virgínia Castro Mendes1, Ricardo Maré2, Vera Cruz e Silva3
1Hospital de Braga, Neuroradiology Department, Braga, Portugal
2Hospital de Braga, Neurology Department, Braga, Portugal
3Medical Image Analysis Center (MIAC), Basel, Switzerland
*Corresponding Author: Mariana Santos, Hospital de Braga, Neuroradiology Department, Braga, Portugal.
Abstract
Homocystinuria is a rare congenital disorder of methionine metabolism characterized by elevated plasma concentration of homocysteine and urine concentration of its oxidation product, homocysteine, most commonly secondary to a deficiency of cystathionine beta-synthase. A 14- year-old girl presented with cerebral venous thrombosis due to classical homocystinuria, whose brain MRI depicted diffuse and bilateral leukoencephalopathy. The genetic study revealed classic homocystinuria (mut C 572 C > T, CBS homozygous gene). A follow-up MRI revealed recovery of white matter appearance and partial permeabilization of venous sinuses.
Keywords: reversible leukoencephalopathy; cerebral venous thrombosis; homocystinuria.
Introduction
Homocystinuria is a rare congenital disorder of methionine metabolism characterized by elevated plasma concentration of homocysteine and urine concentration of its oxidation product, homocysteine, most commonly secondary to deficiency of cystathionine beta-synthase (CBS) [1]. Although not specific, the most common imaging findings include venous thrombosis and multiple cortical and subcortical cerebral infarctions. Diffuse bilateral white matter changes are rarely reported in the literature [2].
Case report
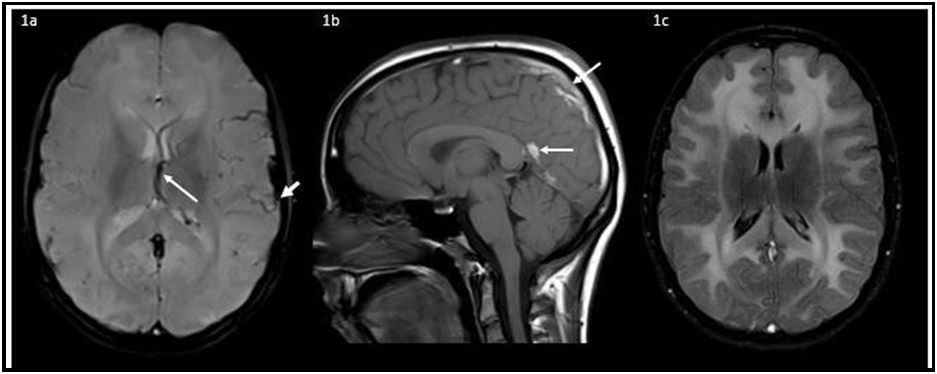
A 14-year-old girl with normal development and no significant past medical history presented with persistent headaches and vomiting. Neurological examination revealed bilateral papilledema. Magnetic resonance imaging (MRI) showed cerebral venous thrombosis and diffuse, bilateral, and symmetrical T2/FLAIR hyperintensity of cerebral white matter (figure 1).
Routine blood studies and thrombophilia screening were unremarkable. Biochemical testing disclosed elevated plasma homocysteine and markedly elevated plasma methionine concentrations (74 μmol/L and 841 μmol/L, respectively). Genetic analysis revealed the homozygous mutation c.572C > T (p.T191M) in the cystathionine beta-synthase gene.
Figure 1. Susceptibility weighted imaging (SWI) sequence showed cerebral venous thrombosisof some cortical veins (figure 1a, small arrow) and the left internal cerebral vein (figure 1a, longarrow), the left transverse, straight and superior sagittal sinuses on sagittal T1-weighted MRI (figure 1b). Fluid attenuation inversion recovery (FLAIR) revealed diffuse, bilateral and symmetrical hyperintensity of cerebral white matter (figure 1c).
She was treated with acetazolamide and unfractionated heparin followed by warfarin. Supplementation with pyridoxine, folic acid, betaine and cystine was initiated, along with dietary restriction.
One year later, follow-up MRI revealed recovery of white matter appearance and partial repermeabilization of venous sinuses (figure 2). At that time, plasma homocysteine was only mildly elevated and methionine concentration was normal.
Figure 2. MRI demonstrated partial repermeabilization of the venous sinuses (2a,b) andcomplete recovery of white matter appearance on FLAIR (2c).
Discussion
Although the diffuse white matter abnormalities could be attributable to venous thrombosis, occurring secondary to poor venous drainage, previous reports suggested a direct role of methionine, an intermediate metabolite that accumulates in classic homocystinuria, as the major contributor [3,4].
Conclusion
In our case, these findings resolved with disease control, even in the absence of total venous repermeabilization, which corroborates this hypothesis.
This unusual imaging presentation of homocystinuria illustrates the importance of considering this entity and other amino-acidopathies in the differential diagnosis of white matter diseases in the pediatric population, as well as associated to venous thrombotic phenomena.
Ethics information
This study complies with the Declaration of Helsinki and was conducted in accordance with the local ethics committee requirements. No figures contain information which allows patient identification, therefore, written patient consent for the publication was not obtained.
Authors’ disclosures: None.
Funding: None.
References
- Li CQ, Barshop BA, Feigenbaum A, Khanna PC (2018) Brain Magnetic Resonance Imaging Findings in Poorly Controlled Homocystinuria. Journal Radiology Case Reports. 12(1):1–8.
- Yaghmai R, Kashani AH, Geraghty MT, Okoh J, Pomper M, et al. (2002) Progressive cerebral edema associated with high methionine levels and betaine therapy in a patient with cystathionine beta-synthase (CBS) deficiency. American Journal Medical Genetics. 108(1): 57–63.
- Sasai H, Shimozawa N, Asano T, Kawamoto N, Yamamoto T, et al. (2015) Successive MRI Findings of Reversible Cerebral White Matter Lesions in a Patient with Cystathionine? – Synthase Deficiency. Tohoku Journal of Experimental Medicine. 237(4): 323–327.
- Vatanavicharn N, Pressman BD, Wilcox WR (2008) Reversible leukoencephalopathy with acute neurological deterioration and permanent residua in classical homocystinuria: A case report. Journal Inherited Metabolic Disease. 31(Suppl 3): 477–481.