Rabia Gilani1, Naima Amir Zaman2, Syed Muhammad Hammad Alam3, Nida Jawad4, Kamal Muhammad Yousuf5, Asif Raza6, Umer Iqbal7*, Muniba Tahir8, Ali Muhammad Saqib9
1Institute: Liaquat National Hospital – Institute for Undergraduate and Postgraduate Medical Studies and Health Sciences, National Stadium Rd, Liaquat National Hospital, Karachi, Karachi City, Sindh 74800.
Affiliation: Department of Vascular Surgery, Liaquat National Hospital – Institute for Undergraduate and Postgraduate Medical Studies and Health Sciences
2Institute: Jinnah Postgraduate Medical Centre (JPMC), Rafique Shaheed Road, Karachi-75510, Pakistan.
3Institute: Liaquat National Hospital – Institute for Undergraduate and Postgraduate Medical Studies and Health Sciences, National Stadium Rd, Liaquat National Hospital, Karachi, Karachi City, Sindh 74800.
Affiliation: Department of Vascular Surgery, Liaquat National Hospital – Institute for Undergraduate and Postgraduate Medical Studies and Health Sciences. ORCID: 0000-0001-6341-1745
4Institute: Liaquat National Hospital – Institute for Undergraduate and Postgraduate Medical Studies and Health Sciences, National Stadium Rd, Liaquat National Hospital, Karachi, Karachi City, Sindh 74800
Affiliation: Department of Gastroenterology, Liaquat National Hospital – Institute for Undergraduate and Postgraduate Medical Studies and Health Sciences 5Institute: Liaquat National Hospital- Institute for Undergraduate and Postgraduate Medical Studies and Health Sciences, National Stadium Rd, Liaquat National Hospital, Karachi, Karachi City, Sindh 74800.
Affiliation: Department of Vascular Surgery, Liaquat National Hospital – Institute for Undergraduate and Postgraduate Medical Studies and Health Sciences 6Institute: Liaquat National Hospital – Institute for Undergraduate and Postgraduate Medical Studies and Health Sciences, National Stadium Rd, Liaquat National Hospital, Karachi, Karachi City, Sindh 74800
Affiliation: Department of Vascular Surgery, Liaquat National Hospital – Institute for Undergraduate and Postgraduate Medical Studies and Health Sciences
7Institute: Shaheed Mohtarma Benazir Bhutto Medical College Lyari, Lyari Hospital Rd, Rangiwara Karachi, Karachi City, Sindh 75010 Affiliation: Sindh Government Lyari General Hospital, Karachi . ORCID: 0000-0004-3392-7192
8Institute: Jinnah Postgraduate Medical Centre (JPMC), Rafique Shaheed Road, Karachi-75510, Pakistan
9Institute: Liaquat National Hospital – Institute for Undergraduate and Postgraduate Medical Studies and Health Sciences, National Stadium Rd, Liaquat National Hospital, Karachi, Karachi City, Sindh 74800
*Corresponding Author: Umer Iqbal, MBBS, Institute: Shaheed Mohtarma Benazir Bhutto Medical College Lyari, Lyari Hospital Rd, Rangiwara Karachi, Karachi City, Sindh 75010. Affiliation: Sindh Government Lyari General Hospital, Karachi. ORCiD: 0000-0004-3392-7192.
Abstract
Arterial thrombosis is a rare extra- intestinal complication of ulcerative colitis with very limited treatment options available for it, since the cause of thrombosis in a patient of ulcerative colitis is not well understood. Many procoagulant factors are believed to be contributing to the thrombus formation. Ulcerative colitis, being an inflammatory disease, activates the coagulation systems which in turn increases the risk of hypercoagulability and thromboembolic events. We, herein, report a case of middle-aged male with ulcerative colitis, presenting in Vascular Surgery clinic with recurrent right acute lower limb ischemia due to femoral artery thrombosis.
Introduction
Inflammatory bowel disease (IBD) constitutes Ulcerative colitis (UC) and Crohn’s disease (CD). Chronic inflammatory bowel diseases, pursue a protracted relapsing and remitting course, usually extending over years. However, the disease in UC is limited to the colon and rectum while CD can involve any part of gastrointestinal tract. Patients diagnosed with UC and diffuse pancolitis often present with a mild inflammatory response in the ileum characterized as backwash ileitis. Furthermore, a significant proportion of UC patients (40-60%) exhibit mild inflammatory involvement of the upper GI tract, highlighting the extracolonic involvement [1]. Ulcerative colitis is a relapsing disorder characterized by attacks of bloody diarrhoea with stringy mucoid material, lower abdominal pain and cramps which are temporary relived by defecation. Though more than half of the patients have clinically mild disease, almost all experience at least one relapse during a10-year period and up to 30% require colectomy within the first 3 years, if disease is in refractory phase. Colectomy effectively cures intestinal disease but extraintestinal manifestation may persist in patients with UC.
Extraintestinal manifestations of inflammatory bowel disease (IBD)affect 25-36% of patients [2]. Common extraintestinal manifestations of UC include migratory polyarthritis, sacroiliitis, ankylosing spondylitis, uveitis and skin lesions [3]. In a few cases limb discoloration secondary to thrombosis can be the first presentation of UC [4]. IBD patients are at a 3-fold increased risk of developing thrombotic complications. More than 60% vascular complications are accounted for peripheral venous thrombosis or pulmonary embolism. Usual sites are portal, mesenteric and cerebral veins [3,5]. More pronounced is venous thromboembolism (VTE) while Arterial Thromboembolism (ATE) is comparatively less in occurrence [5]. Notably, this risk surges to a 15-fold increase during disease flares, making thromboembolism the most dreadful and rarest complication of IBD [6].
Studies have consistently shown that individuals with ulcerative colitis (UC) are at a substantially elevated risk of developing thromboembolic events, with reported prevalence rates ranging from 1.2% to 6.4% (4<3). In the West, the incidence of ulcerative colitis is 10-20 per 100000, with the prevalence of 100-200 per 100000 while the incidence of developing thromboembolic disease in a patient with ulcerative colitis accounts for 50 per 10000-year [1].
The exact pathogenesis behind the development of thrombosis in UC is complex and not fully explained. No definitive cause has been identified so far. However, the thrombotic phenomena are thought to be multifactorial in the inflammatory disease encouraging the pro coagulant state of blood [5].
Case Report
A 56-year-old male patient with no prior comorbid except that he was a known case of UC since 2022, came to the outpatient department (OPD) with a complaint of right lower limb pain and discoloration for 3 days. According to the patient he was in the usual state of health 3 days back when he started having a sudden onset of severe pain in his right leg which failed to subside by over-the-counter medications. He noticed bluish discoloration of the right foot along with weak movement of the foot and numbness. When detailed history was taken, the patient revealed that he had a recent flare of ulcerative colitis a week back, despite being on his routine medications for UC, mesalamine and Steroids. According to the patient he had similar episodes of discoloration and pain, twice in 2023, for which he underwent right femoral artery embolectomy. And at both episodes, he doubted he had a flare of disease, supported by his prescription which included steroids, mesalamine. He was on a low dose anticoagulant, since the last episode of ischemia. At the time of presentation, he was also on low dose steroids for a long time. He had a history of smoking, which he quit when diagnosed with UC. He underwent laparoscopic cholecystectomy in 2004. His past workup revealed persistently raised platelet count of more than 550,000 per cubic millilitre, with remaining workup was almost in normal limits. Clinically he was a healthy-looking man, vitally stable, with BP of 120/85mmHg, 92bpm heart rate but was anxious. His systemic examination was unremarkable with abdomen was soft and non- tender.
On examination for right lower limb revealed, dusky forefoot, cold right leg up to knee with swollen, but soft and mildly tender to touch calf. He had impaired sensation on sole of foot and toes, along with loss of movement on toes. Patient had palpable normovolumic femoral pulse while rest of the distal pulses were not appreciated (popliteal, posterior tibial, and dorsalis pedis). Handheld Doppler though gave monophasic signals in distal pulses. According to Rutherford classification (Table 01) of arterial thrombosis patient was in stage II b.
Table 01: Rutherford’s classification for acute limb ischemia
|
Category |
Clinical Findings |
Limb viability |
Treatment |
|
Category I |
1. Doppler signals: Arterial / venous: audible 2. Sensory intact 3. Motor intact 4. Acute onset of pain; may or may not have rest pain in extremity |
Viable |
Tx: embolectomy (<48hr) |
|
Category II a |
1. Doppler signals: Arterial: often inaudible Venous: audible 2. Decreased sensation 3. Motor intact 4. Rest pain in extremity |
Marginally threatened |
Urgent embolectomy (<24hr) |
|
Category II b |
1. Doppler signals: Arterial: usually inaudible Venous: audible 2. Decreased sensation 3. Decreased motor strength. 4. Rest pain in extremity |
Immediatel y threatened |
Immediate embolectomy: time is of the essence and the limb is still salvageable (<4hr) |
|
Category III |
1. Doppler signals: Arterial: inaudible Venous: inaudible (thrombosis in venous system secondary to stagnant flow) 2. No sensation in limb 3 No motor strength in limb |
Nonviable irreversible |
Amputation; non salvageable limb. Do not attempt revascularization as ischemic tissue could release toxins leading to cardiac arrest. |
Laboratory Findings And Intervention:
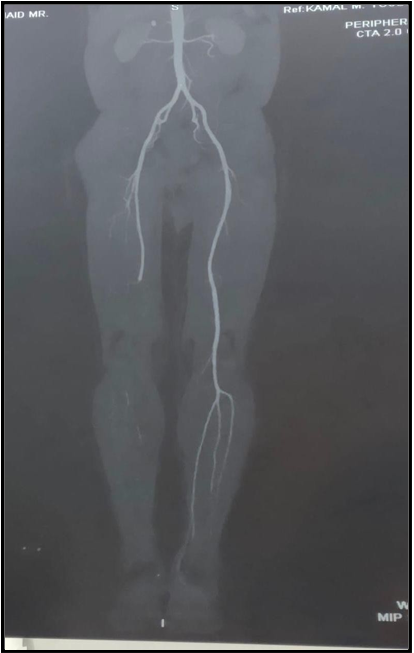
On admission his workup showed haemoglobin of 8.22g/dl and platelet count of 609,000 per cubic millilitre with elevated ESR (erythrocyte sedimentation rate). The rest of his haematological parameters were with in normal limits, including coagulation profile. CT angiogram of lower limb was done and showed thrombosis of the right distal superficial femoral artery including the right popliteal and distal axial arteries (Figure 01). Immediate intervention was planned, after counselling of patient and his family. On embolectomy, multiple clots were retrieved from the right femoro-popliteal segment of artery. The patient was transfused with 1 packed red blood cells. Patient tolerated the procedure well and his condition improved. After one night stay at the hospital patient was discharged on anticoagulant enoxaparin subcutaneously, according to the weight, twice daily for 3 months, antibiotic and analgesic cover was given, along with Gastroenterologist follow up, to avoid exacerbation of UC.
Figure 01: CT ANGIOGRAM of lower limb; showing failure of right distal femoral artery, Popliteal artery and distal branches to opacify.
Discussion
In 1936 Bargen and Barter in their study described the association between inflammatory bowel disease (IBD) and thromboembolism, since then numerous cases and studies have shown the possible link between the two pathologies (inflammation and thrombosis).
Chronic inflammation is associated with multiple risk factors which could become the cause of thrombotic events in patients with IBD, and so in UC. In the complex mechanisms of thrombus formation, it’s not only the genetic predisposition, but also factors such as such endothelial disruption attracting leukocytes and platelets, release of TNF-alpha, Interleukin-1 and even bacterial lipopolysaccharide which triggers the coagulation cascade, either intrinsic or extrinsic pathway [5,7]. This further augments levels of von Willibrand factors, factor VIII and fibrinogen, this effect gets a boost with low levels antithrombin factors such as antithrombin III and protein S in serum and so generates and propagates a thrombus [2,10, 12, 13].
Besides inflammatory factors, in UC, role of gut microbiome believes to be crucial in thrombogenesis. As normal commensals get altered and so as permeability of gut in inflammatory phase, encouraging pathogenic organism like gram negative Enterobacteriaceae (Entero) family, contributing to thrombosis via intrinsic pathway [7]. Also, numerous studies have shown a link of major pro-thrombotic genetic predispositions and IBD. According to recent research it has been observed that patients with inherited bleeding and coagulations disorders such as haemophilia A and B, von Willebrand disease has increased tendency to develop thromboembolic complications [8]. Adding to these, the role of steroids, either low or high dose, cannot be ignored, as literature shows that corticosteroids when used for a longer time or on a high dose, not only increases thrombin generation but also increases VWF gene transcription [10,11]. Though studies suggests that it’s not the secretion, but VWF gene transcription which is accelerated, and so binding with the Factor VIII, which encourages adhesion of platelets and so the formation of clot [11]. The detailed summary of conducive risk factors of thrombosis in IBD is illustrated in Figure 02.
Figure 02: Comprehensive summary of causative risk factors of thrombosis in IBD
The following case of recurrent femoral artery thrombosis highlights a rather rare extra-intestinal manifestation of UC, in ex-smoker patient who had a recent history of severe acute flare of disease and was being treated with steroids. All this adequately leads to formation of thrombus even through the patient was on antithrombin therapy. Interestingly in our patient the platelet count was found to be persistently high since he was diagnosed with UC, that is more than 550,000 per cubic millilitre, even with the treatment after acute remission of disease.
Hypercoagulable status in our patient was likely also supported by history of chronic smoking, which could have predisposed patient's chronically diseased vascular channels to thrombotic events. This haemostatic shift to procoagulant state in IBD, is therefore a complicated process and gets more complex as the disease advances or during acute flares. Such patients require urgent intervention when comes a limb threatening situation. Thus, in short, in patients with IBD, extra intestinal manifestation can present with signs and symptoms of thromboembolism, either arterial or venous. Initial screening via US Doppler can detect peripheral arterial and venous thrombosis, while a definitive diagnosis can be made with a CT Angiogram [4,6].
Management certainly requires a teamwork including Vascular Surgeon and Gastroenterologist. Treatment modalities for limb threatening ischemia include medical and surgical approaches. Patients are usually put on low molecular weight heparin, but surgical approaches remain the treatment of choice. Arterial thrombosis can usually be treated by thrombectomy, embolectomy and compartment fasciotomy in patients with limb ischemia. Research suggests that patients diagnosed with IBD such as UC had a very high risk of having thrombosis within 5 years after discontinuing anticoagulant therapy as prophylaxis. Moreover, IBD itself is associated with a 2.5 times increased risk of unprovoked VTE recurrence. Another study held by Canadian society of gastroenterology recommends that anti coagulation therapy should be given as prophylaxis to the patient of ÜÇ who had underwent any recent surgery, recent flare or simply had a history of recurrent arterial and venous thrombosis [6].
Arterial thromboembolism (ATE) is much rarer than venous thromboembolism (VTE) in IBD due to the pathophysiology of the disease. In spite, there are some cases of ATE in patients with IBD with involvement of thrombosis or occlusion concurrently or separately of the upper and lower extremity [14], aorta [15], coronary [16], carotid [17], splanchnic [18] and cerebral [19] arteries. Our case of recurrent femoral artery thrombosis in a patient with UC is much rare and have not been reported yet, however there is a case in literature, of a 49-year-old woman diagnosed with UC in 2010 who suddenly started having pain and sensory symptoms of both of her lower limbs in June 2015 and her MRA showed no signs of blood flow in the distal femoral artery [12]. She started anticoagulation therapy and later arterial thrombectomy with Fogarty's ballon catheter was performed which relieved her severe pain and she was discharged after 28 days from the admission. When comparing with the case reported by Mimari Kanazawa [12], patient in our case reported with pain and discoloration of right lower limb for the 3rd time despite having right femoral artery embolectomy and anticoagulant therapy. This recurrent presentation makes our case distinctive and worthy. Another case by DA Mikroulis [20] on thrombosis of the brachial and radial artery in concordance with UC was published in 1999 in a 43- year-old man who was having recurrent symptoms even after attempts to reinstate the blood flow and the last efficacious remedy was the resection of the large bowel. In collation, the patient in our case had thrombosis of right femoral artery and its territories with bluish discoloration of his right lower limb which was treated with removal of multiple clots from the femoral artery and its branches. This also makes our case peculiar and notable.
Conclusion
Since femoral artery thrombosis in patients with UC, leading to limb ischemia is not common, this case invoked a curiosity as it was a recurrent episode, even though patient was on low dose anticoagulant. The strong procoagulant activity, which seems to be accelerating after every flare and in combination with steroids, suggests that the shift to a hypercoagulable state in IBD has yet to unveil a lot more reasoning for thrombosis. Further research and studies are required to obtain a better correlation between the current regimen and its effects on thromboembolic events.
Statement and declaration:
Ethical Approval: Our institution doesn’t require ethical approval for the case report, however written consent was taken from the patient
Competing interests: None
Authors’ contributions: RG and AR collected the data material, NAZ, and MT did the writing of the manuscript, RG did the referencing, KMY and SMHA did the supervision, and review, NJ and AMS put insights from the Gastroenterology point of view, UI did the writing part in discussion, review, editing and corresponding of the manuscript.
Funding: None
Availability of data and materials: All data of the correspondence is publicly available on databases such as PubMed and Google scholar.
References
- Rosen MJ, Dhawan A, Saeed SA (2015) Inflammatory Bowel Disease in Children and Adolescents. JAMA Pediatr. 169(11): 1053-60.
- Jain S, Bhatt P, Muralikrishna GK, Malhotra P, Kumari S, et al. (2005) Extensive arterial and venous thrombosis in a patient with ulcerative colitis a case report. MedGenMed. 7(2): 10.
- Kalwar HA, Shaikh T, Baloch MH (2021) Concurrent Arterial and Venous Thrombosis in a Patient with Ulcerative Colitis in Remission Phase. J Coll Physicians Surg Pak. 31(2): 215-217.
- Hosseini S.M.V, Foroutan H.R, Sabet B, Nasibi M, Banani S.A (2015) Limb Loss Caused by Thrombosis led to the Diagnosis of Ulcerative Colitis. Iranian Journal of Medical Sciences. 35(1): 69- 71.
- Stadnicki A, Stadnicka I (2021) Venous and arterial thromboembolism in patients with inflammatory bowel diseases. World J Gastroenterol. 27(40): 6757-6774.
- Singh H, Ish P, Dewan R, Anuradha S, Singla S (2016) Combined Arterial and Venous Thrombosis in Ulcerative Colitis- A Rare Vascular Manifestation. J Clin Diagn Res. 10(4): OD12-3.
- Hasan RA, Koh AY, Zia A (2020) The gut microbiome and thromboembolism. Thromb Res. 189: 77-87.
- Giannotta M, Tapete G, Emmi G, Silvestri E, Milla M (2015) Thrombosis in inflammatory bowel diseases: what’s the link? Thrombosis J. 13: 14.
- Zizi O, Benfor B, Jiber H, Bouarhroum A (2016) Embolic lower limb ischemia as a rare complication of ulcerative colitis: A case report and literature review. Journal des Maladies Vasculaires. 41(4): 279-285.
- Cong Dai, Min Jiang, Qin Cao, (2018) Steroids and the Risk of Venous Thromboembolic Events in Inflammatory Bowel Disease, Journal of Crohn's and Colitis. 12(5): 627.
- Majoor CJ, Sneeboer MM, de Kievit A, Meijers JC, van der Poll T, et al. (2016) The influence of corticosteroids on hemostasis in healthy subjects. J Thromb Haemost. 14(4): 716-23.
- Kanazawa M, Sugaya T, Takahashi F, Takenaka K, Tsuchida K, et al. (2020) A Case of Bilateral Acute Inferior Limb Ischemia in a Patient with Ulcerative Colitis. Clin Med Insights Case Rep. 13: 1179547620912734.
- Al Ghadeer HA, Alsalman SA, Alobaid J, AlAbdi ZI, Aljereish SS, et al. (2022) Cerebral Venous Sinus Thrombosis is a Reversible Complication of Ulcerative Colitis. Cureus. 14(3): e23099.
- Haumer M, Teml A, Dirisamer A, Vogelsang H, Koppensteiner R, et al. (2007) Severe ulcerative colitis complicated by an arterial thrombus in the brachiocephalic trunk. Inflamm. Bowel Dis. 13(7): 937–938.
- Novacek G, Haumer M, Schima W, Müller C, Miehsler W, et al. (2004) Aortic mural thrombi in patients with inflammatory bowel disease: Report of two cases and review of the literature. Inflamm. Bowel Dis. 10(4): 430–435.
- Mutlu B, Ermeydan CM, Enç F, Fotbolcu H, Demirkol O, et al. (2002) Acute myocardial infarction in a young woman with severe ulcerative colitis. Int. J. Cardiol. 83(2): 183–185.
- Prior A, Strang FA, Whorwell PJ (1987) Internal carotid artery occlusion in association with Crohn’s disease. Dig. Dis. Sci. 32(9): 1047–1050.
- Irving PM, Alstead EM, Greaves RR, Feakins RM, Pollok RC, et al. (2005) Acute mesenteric infarction: An important cause of abdominal pain in ulcerative colitis. Eur. J. Gastroenterol. Hepatol. 17(12): 1429–1432.
- Katsanos AH, Kosmidou M, Giannopoulos S, Katsanos KH, Tsivgoulis G, et al. (2014) Cerebral arterial infarction in inflammatory bowel diseases. Eur. J. Intern. Med. 25(1): 37–44.
- Mikroulis DA, Antypas GD, Fournogerakis SD, Antoniadis PN, Rigas AM (1999) Arterial Thrombosis in Ulcerative Colitis: Case Report. Int J Angiol. 8(1): 62-64.