Tahir Buranˡ*, Semin Ayhan²
ˡDepartment of Gastroenterology, Manisa Celal Bayar University Faculty of Medicine, Manisa, Turkey. Orcid 0000-0002-8077-2582
²Department of Pathology, Manisa Celal Bayar University Faculty of Medicine, Manisa, Turkey
*Corresponding Author: Tahir BURAN, Department of Gastroenterology, Manisa Celal Bayar University Faculty of Medicine, Manisa, Turkey. Orcid 0000-0002-8077-2582
Abstract
Malignant melanoma is responsible for 1–3 % of all malignancies, and the gastrointestinal tract is one of the most common metastatic locations. Malignant melanoma is a very aggressive type of cancer; some patients have distant metastasis at presentation. Gastrointestinal system metastases are common and generally asymptomatic. The disease is rarely diagnosed only by gastrointestinal symptoms. Our case was diagnosed with malignant melanoma after upper gastrointestinal bleeding. Characteristic lesions for malignant melanoma were seen by gastroscopy. The diagnosis was confirmed by biopsy.
Keywords: Malignant melanoma, gastrointestinal bleeding, gastric metastasis
Introduction
Malignant melanoma (MM) is responsible for 1–3% of all malignancies, with the gastrointestinal tract one of the most common metastatic locations [1].
MM is one of the most aggressive and highly malignant skin tumors with continuously increasing incidence [2]. Malignant melanoma frequently spreads to the gastrointestinal tract. Only 1–4 % of melanoma metastases to the gastrointestinal tract are detected. Gastrointestinal system metastases often happen, most of which are asymptomatic [3]. Gastrointestinal system metastases are observed at a rate of 60 % in the autopsy series of patients with malignant melanoma [4]. Abdominal pain, anemia, and rarely melena is noted in patients with symptomatic gastrointestinal metastases [5]. Here, we present a case diagnosed with malignant melanoma and consequently admitted with abdominal pain and melena.
Case
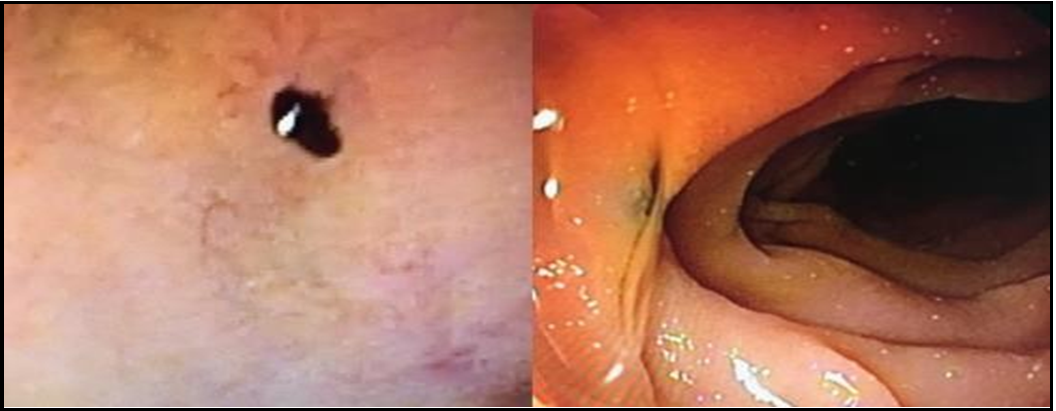
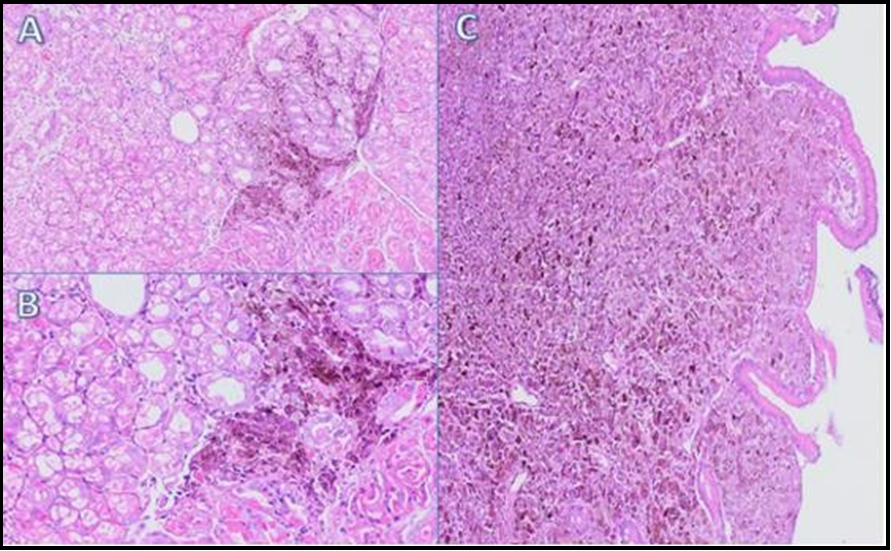
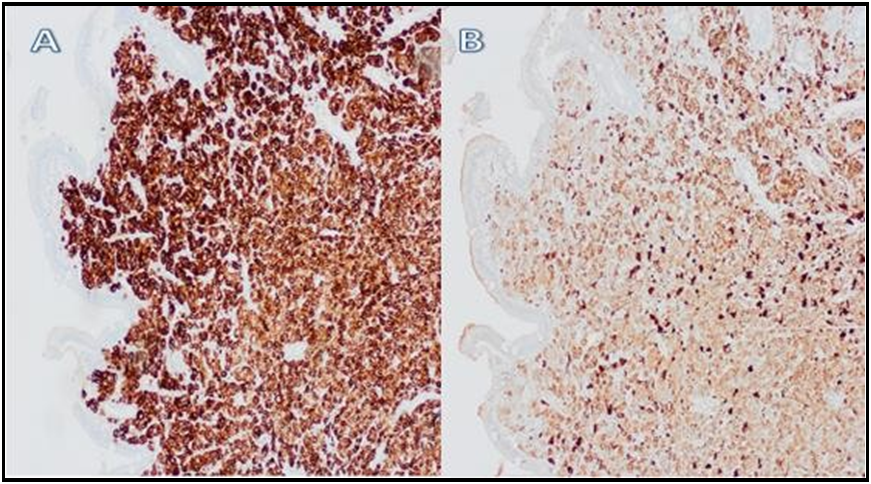
A 75-year-old female patient presented to the gastroenterology outpatient clinic with abdominal pain and melena symptoms. She had no history of a known co-morbidity and had a history of a nevus excision on the left side of her face 2 years ago, the pathology of which was considered to be intradermal nevus. Her hemoglobin level at baseline was 10.5 g/dl, hematocrit was 32.7 %, platelet count was 205 x 103 µL, urea was 35 mg/dl, creatin was 1 mg/dl, alanine aminotransferase (ALT) was 18 U/L, aspartate transaminase (AST) was 27 U/L, alkaline phosphatase (ALP) was 218 U/L, lactate dehydrogenase (LDH) was 746 U/L. The patient underwent endoscopy and colonoscopy during the same session. Diffuse ulcers and black-pigmented lesions were detected in the stomach and duodenum during the endoscopy (Figures. 1,2). Biopsies were performed on the lesions. Biopsy specimens revealed tumoral cells especially diffuse in lamina propria, with brown-black pigment accumulation in the cytoplasm and large vesicular nuclei with marked atypia. Tumor cells were positive for S100, HMB45, and Melan A (Figures. 3,4). The present findings were suggestive of duodenal and gastric metastases of malignant melanoma. The patient underwent a colonoscopy, and average colonoscopic results were observed. The patient was referred to the oncology clinic to investigate the primary tumor and plan the treatment.
Figure 1:
Figure 2:
Figure 1&2: Diffuse ulcers and black-pigmented lesions were detected in the stomach and duodenum during the endoscopy
Figure 3:
Figure 4:
Figure 3&4: Tumor cells were positive for S100, HMB45 and Melan A
Discussion
Malignant melanomas are malignant tumors arising from the skin cells called melanocytes [6]. Its incidence is 3.4 % among all cancers [7], and its prognosis is generally poor. Stage 4 malignant melanoma patients' five-year survival rate was only 14 % [8].
Excisional biopsy is still the golden standard for diagnosis [9]. Various morphologic variants of malignant melanoma make pathologic diagnosis extremely difficult [10], and accurate pathologic diagnosis is essential for early diagnosis and treatment.
Malignant melanoma can metastasize to all organs, but it is primarily known to metastasize to the gastrointestinal system frequently [11]. The gastrointestinal system metastasizes most frequently to the small and large intestines and anorectal areas. Gastric metastasis is known to be very rare [12]. However, there were metastases to the stomach and duodenum in our case.
Gastrointestinal melanomas are frequently characterized by non-specific symptoms and signs like abdominal pain, nausea, dysphagia, upper and lower GIS bleeding, and melena [13]. Abdominal pain, anemia, and melena were reported in our case.
Endoscopic evaluation has an essential place in the diagnosis of gastrointestinal system melanoma. Black-pigmented lesions, submucosal nodules, ulcerated lesions, and masses with polypoid structures can be detected with endoscopy. Bull's eye appearance in the lesion is characteristic of barium analyses [14]. In our case, numerous, black-pigmented nodular lesions and necrotic ulcers were detected in the endoscopic examination.
Conclusion
Malignant melanoma is an aggressive tumor that can rapidly metastasize. Therefore, early diagnosis and treatment are essential. If non-specific gastrointestinal symptoms and signs occur in diagnosed patients, it should be remembered that it could be a GIS metastasis, and endoscopic evaluation should be considered.
Declarations
Funding: Not applicable
Conflicts of interest/Competing interests: there is no conflict of interest.
Availability of data and material: All data are available in the archive of "Manisa Celal Bayar University Faculty of Medicine."
Code availability: Not applicable
Ethics approval: Ethical approval was obtained from the patient.
Consent to participate: Approved to participate.
Consent for publication: Approved to publication.
References
- Silva S, Tenreiro N, Melo A, Lage J, Moreira H, et al. (2018) Metastatic melanoma: An unusual cause of gastrointestinal bleeding and intussusception—A case report. Int J Surg Case Rep. 53: 144–146.
- Situm M, Buljan M, Kolić M, Vučić M (2014) Melanoma– clinical, dermatoscopical, and histopathological morphological characteristics. Acta Dermatovenerol Croat. 22(1): 1–12.
- Falk V, Zepeda-Gomez S, Sultanian R, Kohansal-Vajargah A (2018) Acute upper gastrointestinal bleeding in a patient with malignant melanoma. BMJ Case Rep. 2018: bcr2018225869.
- Genova P, Sorce M, Cabibi D, Genova G, Gebbia V, et al. (2017) Gastric and Rectal Metastases from Malignant Melanoma Presenting with Hypochromic Anemia and Treated with Immunotherapy. Case reports in oncological medicine. 2017: 2079068.
- Sundersingh S, Majhi U, Chandrasekar SK, Seshadri RA, Dakshinamurthy SK, et al. (2012) Metastatic malignant melanoma of the small bowel–report of two cases. J Gastrointest Cancer. 43(2): 332-5.
- Kozovska Z, Gabrisova V, Kucerova L (2016) Malignant melanoma: diagnosis, treatment and cancer stem cells. Neoplasma. 63(4): 510-7.
- GLOBOCAN (2020) Global Cancer Observatory.
- Alvarado-Cabrero I, Estévez-Castro R, Valencia-Cedillo R (2019) [Metastasis of melanoma to the gastrointestinal tract. Report of three cases]. Rev Med Inst Mex Seguro Soc. 57(1): 42– 47.
- Pavri SN, Clune J, Ariyan S, Narayan D (2016) Malignant Melanoma: Beyond the Basics. Plast Reconstr Surg. 138(2): 330e-340e.
- Brenn T (2015) [Histological spectrum of malignant melanoma]. Pathologe. 36(1): 53–61.
- Liang KV, Sanderson SO, Nowakowski GS, Arora AS (2006) Metastatic malignant melanoma of the gastrointestinal tract. Mayo Clin Proc. 81(4): 511-6.
- El-Sourani N, Troja A, Raab HR, Antolovic D (2014) Gastric Metastasis of Malignant Melanoma: Report of a Case and Review of Available Literature. Viszeralmedizin. 30(4): 273–5.
- Mikkelsen LH, Larsen AC, von Buchwald C, Drzewiecki KT, Prause JU, et al. (2016) Mucosal malignant melanoma - a clinical, oncological, pathological and genetic survey. APMIS. 124(6): 475–86.
- Kotteas EA, Adamopoulos A, Drogitis PD, Zalonis A, Giannopoulos KV, et al. (2009) Gastrointestinal bleeding as initial presentation of melanoma of unknown primary origin: report of a case and review of the literature. In Vivo. 23(3): 487- 9.