K.A.C.C Pemasiri1,2, C.N. Wijesinghe1, S. Mendis1, M.F.M. Makarim1, R.L. Malavige1, M.N.N. Masaima1, P.I. Jayasekera3*, N.S. Chandrasiri1
1Colombo South Teaching Hospital, Kalubowila, Sri Lanka
2Department of Medical Microbiology, Faculty of Medicine, University of Kelaniya, Sri Lanka
3Medical Research Institute, Colombo 08, Sri Lanka
*Corresponding Author: P.I. Jayasekera, Medical Research Institute, Colombo 08, Sri Lanka.
Abstract
Mucormycosis is a rapidly invasive fungal infection common among the immunocompromised population. Pulmonary mucormycosis is a rare and severe form of this condition.
A 32-year-old acutely ill male was found to be in diabetic ketoacidosis on presentation to the hospital. In addition, initial examination and chest radiography findings suggested an infective focus in the lungs. Bronchoalveolar lavage fluid obtained by subsequent bronchoscopy examination yielded Rhizopus species in culture. High-resolution computed tomography of the chest revealed the presence of a ‘Bird’s nest sign’ which is suggestive of invasive fungal infections in the lungs. Although he was started on intravenous amphotericin B, owing to adverse effects, treatment had to be withheld after seven days. His condition gradually deteriorated, and he succumbed to death two days later.
This case emphasizes the importance of having a high degree of suspicion for fungal infection in vulnerable patients and early administration of antifungal therapy.
Keywords: pulmonary mucormycosis, diabetes, bird’s nest sign, Rhizopus, amphotericin B
Introduction
Mucormycosis is an angioinvasive fungal infection caused by members of the order Mucorales. It is common among immunocompromised populations and has significant morbidity and mortality. Several forms of the infection include rhinocerebral, pulmonary, cutaneous, gastrointestinal, and disseminated form. We report on a case of pulmonary mucormycosis (PM), a relatively uncommon form of the infection, in a young male.
Case History
A 32-year-old male with a history of diabetes presented to the Emergency Department with acute onset altered level of consciousness and generalized body weakness. Two weeks before this presentation, he was admitted to a local hospital and treated as for bacterial pneumonia. A chest x-ray taken at that time shows a small opacity near the right hilar region. Despite being discharged from there after three days of intravenous antibiotic treatment, he has continued to be unwell at home. He is a timber mill worker who regularly smokes and uses alcohol and cannabis.
At the time of admission, he looked emaciated and was drowsy. His body temperature was recorded as 99°F and his oxygen saturation level was low. Systemic examination was unremarkable except for crackles in bilateral lungs. Initial investigations revealed him to be in diabetic ketoacidosis. Subsequent investigations revealed a C- reactive protein level of 445 mg/L, a high white cell count, and HbA1c of 16.3%.
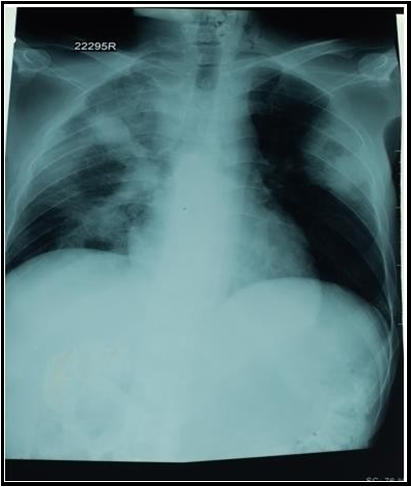
He was transferred to the medical intensive care unit on the same day as his condition was deteriorating. Chest X-ray taken on admission suggests an infective cause involving multiple lobes and cavity formation in both lungs (Figure 1). Chest X-ray taken on the following day shows a rapid progression of the infection. This was further confirmed by a subsequent High-resolution computed tomography (HRCT) of the chest which showed features of necrotizing pneumonia affecting both lungs along with cavity formation.
Ensuing bronchoscopy examination revealed plenty of thick white secretions and bronchoalveolar lavage (BAL) fluid was collected for further investigations. A direct smear of BAL, performed in the hospital microbiology laboratory, was filled with pus cells but no bacteria could be seen. On suspicion of a fungal infection, oral voriconazole was added to his therapy. On the following day, BAL culture had a significant growth of fungus, most likely belonging to the Mucorales order. Therefore, voriconazole was omitted, and intravenous (IV) amphotericin B was started. Given the extensiveness of the infection and the instability of his condition, surgical resection was not a treatment option for him. Another BAL specimen was sent to the Mycology Reference Laboratory, where broad, aseptate fungal filaments were visualized on direct microscopic examination. Later on, Rhizopus species were isolated from culture (Figure 2). A review of the HRCT revealed the presence of a ‘bird’s nest’ sign. Further radiological examinations did not detect any abnormalities in orbits or paranasal sinuses.
By the third day of IV amphotericin B therapy, haematological indices and serum potassium levels started dropping accompanied by a general deterioration in his condition. Due to persistent derangement in cell lines and electrolytes, IV amphotericin B had to be withheld on the seventh day of therapy. Despite all efforts, the patient became haemodynamically unstable and succumbed to death two days later.
Figure 1: Chest x-ray on day 1.
Figure 2: Rhizopus species with prominent rhizoid (arrow). (Lactophenol cotton blue stain).
Figure 3: Bird's nest sign ( arrow).
Discussion
Mucormycosis is a rapidly progressive fungal infection caused by filamentous fungi in the subphylum Mucormycotina, order Mucorales. [1,4] They are commonly found in decaying food and outdoor environments. [1] Rhino-orbital-cerebral mucormycosis is the most common disease manifestation, followed by cutaneous and pulmonary mucormycosis. [2] The usual route of infection is by inhalation of spores. [2] Most cases of mucormycosis are caused by members belonging to the Rhizopus and Mucor genera. [1]
It is an infection common among immunocompromised populations. Poorly controlled diabetes is the most common underlying condition, and a substantial proportion of patients have documented ketoacidosis at presentation. [1-3] This patient was in a significant immunosuppressed state due to poorly controlled diabetes. Regular alcohol and substance abuse leading to poor nutrition were added risk factors. He may have acquired the infection from the sawmill he worked at, as these fungi are frequently found in the outdoor environment.
Pulmonary mucormycosis has non-specific symptoms and the median time between first symptoms and diagnosis is about two weeks. [6] Given the history of prior hospital admission and continued unwellness, it is likely that he has been harboring the illness since the initial admission. Although rhino-cerebral mucormycosis is the most common form of infection in patients with uncontrolled diabetes, chronic lung damage caused by smoking, cannabis abuse and exposure to sawdust may have predisposed him to develop pulmonary disease instead. In keeping with the epidemiology of PM, he presented with advanced disease not amenable to surgical resection. Therefore, the main components of management in this case were prompt anti-fungal therapy and optimization of underlying medical conditions. Development of blood dyscrasias and electrolyte imbalances are well-known side effects of IV amphotericin B treatment.
Lobar and segmental consolidations on chest imaging are common nonspecific findings that can rapidly progress if left untreated. Due to the angioinvasive nature of Mucorales, necrosis is another frequent finding. A bird’s nest sign is seen when irregular, intersecting areas of stranding and irregular lines are present within an area of ground glass opacity. [7] It favors pulmonary mucormycosis over invasive Aspergillus infections. [1]
Members of the Mucorales order are characterized by rapid macroscopic growth and microscopic features of broad aseptate fungal filaments. Early presumptive laboratory identification led to the early administration of definitive antifungal therapy in this patient. About half of the patients with PM die within 90 days of diagnosis, and fatal outcomes are common in patients with prolonged neutropoenia and empirical voriconazole use. [2-4] Therefore, caution is needed in using voriconazole even in patients with prior histories of invasive pulmonary aspergillosis, in whom PM cannot be ruled out initially.[3]
This case report highlights the importance of having a high level of suspicion for fungal infection in at-risk patients and early administration of antifungal therapy.
Statement on conflict of interest: There are no conflicts of interest.
Acknowledgments / Funding source: This case report was not funded by any external organization.
References
- Agrawal R, Yeldandi A, Savas H, Parekh ND, Lombardi PJ, et al. (2020) Pulmonary mucormycosis: risk factors, radiologic findings, and pathologic correlation. Radiographics. 40(3): 656- 666.
- Jeong W, Keighley C, Wolfe R, Lee WL, Slavin MA, et al. (2019) The epidemiology and clinical manifestations of mucormycosis: a systematic review and meta-analysis of case reports. Clinical microbiology and infection. 25(1): 26-34.
- Son HJ, Song JS, Choi S, Jung J, Kim MJ, et al. (2020) Risk factors for mortality in patients with pulmonary mucormycosis. Mycoses. 63(7): 729-736.
- Serris A, Danion F, Lanternier F (2019) Disease entities in mucormycosis. Journal of Fungi. 5(1): 23.
- Hammer MM, Madan R, Hatabu H (2018) Pulmonary mucormycosis: radiologic features at presentation and over time. American Journal of Roentgenology. 210(4): 742-747.
- Legouge C, Caillot D, Chrétien ML, Lafon I, Ferrant E, et al. (2014) The reversed halo sign: pathognomonic pattern of pulmonary mucormycosis in leukemic patients with neutropenia. Clinical infectious diseases. 58(5): 672-8.
- Nimesh R, Vyas S (2018) Chest CT Scan Signs: A Few Noteworthy Additions. Chest. 153(6): 1516-1517.