Juzaily Fekry Leong*, Teh Jun Xian, Azizi Zainodin, Levin Kesu Belani, Mohammed Ashraff, Mohd Ariff, Sabarul Afian Mokhtar
Department of Orthopaedic and Traumatology, Faculty of Medicine, Hospital Canselor Tuanku Muhriz, Cheras, Kuala Lumpur, MYS
*Corresponding Author: Juzaily Fekry Leong, Department of Orthopaedic and Traumatology, Faculty of Medicine, Hospital Canselor Tuanku Muhriz, Cheras, Kuala Lumpur, MYS
Abstract
Introduction: Patients who sustain an osteoporotic fracture are at increased risk of sustaining another fracture hence efforts are directed towards secondary fracture prevention. The aim of this study was to identify the osteoporosis care gap in patients admitted with fragility fractures in University Kebangsaan Malaysia Medical Centre (UKMMC).
Methods: Patients admitted to a tertiary care hospital with fragility fractures were identified from the admission registry from January 2016 to December 2016. The demographic data and drug prescriptions related to osteoporosis treatment were obtained upon discharge.
Results: A total of 207 patients (85 male and 122 female) were identified with fragility fractures. Majority sustained hip fractures (n=141, 68.1 %), followed by vertebrae fractures (n=43, 20.8 %) and wrist fracture (n=23, 11.1%). Patients were prescribed calcium (n=113, 54.6 %) and vitamin D (n=89, 43.0 %). Only 40 (19.3 %) patients were given anti-osteoporotic drugs within 6 months of discharge.
Conclusion: Persistent care gap exists for people suffering fragility fractures caused by osteoporosis. Greater awareness among doctors in managing osteoporosis among patients with fragility fracture to prevent secondary fracture. Improvement of fracture care can be achieved by implementing a Fracture Liaison Service program in the hospital setting.
Keywords: Care Gap, Fragility Fracture, Osteoporosis
Introduction
Osteoporosis is defined as deterioration in bone and architecture resulting in weakness of the bone, which is then prone to fracture. It is one of the major non-communicable diseases, accounting for 0.83% of the global burden worldwide [1]. The prevalence of osteoporosis and its consequences (i.e fragility fractures) is increasing worldwide in parallel with global population aging. Patients, who sustain a fragility fracture after the age of 50 years are at higher risk of getting subsequent fractures by 2- to 9- fold [2].
Efforts and measures should be taken to prevent subsequent fractures as these are associated with a greater increase in mortality rates and a significantly higher cost. International guidelines for secondary prevention of fragility fractures are available, which include pharmacological therapy to treat osteoporosis and giving supplements to promote bone health [3]. Medications are now available for the prevention and treatment of osteoporosis. These are known to have a beneficial effect on bone mineral density (BMD) and reduce the risk of fracture [4]. Other methods include assessing osteoporosis, strategies for fall prevention in the elderly, and avoiding tobacco and excessive alcohol intake.
Treatment of osteoporosis following osteoporotic fractures is widely variable, but generally rather poor. A Belgium study has shown treatment rates of osteoporosis following fractures were as low as 6 % [5]. In the study involving patients of multiple Asian countries, only 33 % of patients were given medication for osteoporosis after hospitalization for a hip fracture [6]. Our study aimed to identify the osteoporosis care gap in patients admitted with fragility fractures in University Kebangsaan Malaysia Medical Centre (UKMMC).
Method
This was a retrospective review of hospital records of patients treated in a tertiary care hospital with fragility fractures from January 2016 to Dec 2016. Patients above 49 years of age and sustained hip, wrist, or vertebrae fractures following a fall from standing height (fragility fracture) are included. Diagnosis of patients was obtained in admission records from orthopedic wards. The demographic data such as age, gender, ethnicity, and drug prescriptions related to osteoporosis treatment were obtained upon discharge and on follow-up, up to 6 months after patients sustained a fragility fracture. A patient who has a bone mass density (BMD) scan requested within 6 months after diagnosis was also recorded from their appointment records in the hospital computer system.
Result
A total of 207 patients (85 male and 122 female) were identified with fragility fracture (Table 1). The commonest age group were those between 70 to 79-years of age (Figure 1 & 2). Majority sustained hip fractures (n=141, 68.1 %), followed by vertebrae fractures (n=43, 20.8 %) and wrist fracture (n=23, 11.1 %). 24 (11.6 %) patients only have Bone Mass Density requested within six months of diagnosis. For those who have sustained fragility fracture, 69 (11.8 %) of patients have a previous history of fracture. In term of osteoporotic management, our patients were prescribed with calcium (n=113, 54.6 %) and vitamin D (n=89, 43.0%) within 6 months after diagnosis. Only 40 (19.3 %) patients were given anti-osteoporotic drugs after 6 months of diagnosis. The most common comorbid among patients were hypertension (n= 134, 64.7 %) followed by diabetes mellitus (n= 92. 44.4 %), and dyslipidemia (n= 36, 17.4 %), (Figure 3)
Table 1: Demographic profile: Total patients admitted (N = 207)
|
Demographic Profile |
Frequency (N) |
Percentage (%) |
|
Age (mean ± SD) |
73.0 ± 10.7 |
|
|
Age Group 50-54 55-59 60-64 65-69 70-74 75-79 80-84 85-89 90-94 >94 |
10 16 20 30 36 39 23 20 9 4 |
4.8 7.7 9.7 14.5 17.4 18.8 11.1 9.7 4.3 1.9 |
|
Gender Male Female |
85 122 |
41.1 58.9 |
|
Ethnics Malay Chinese India |
64 128 15 |
30.9 61.8 7.2 |
|
Managements (Yes) Calcium Vitamin D Anti-osteoporosis Bone mineral density |
113 89 40 24 |
54.6 43.0 19.3 11.6 |
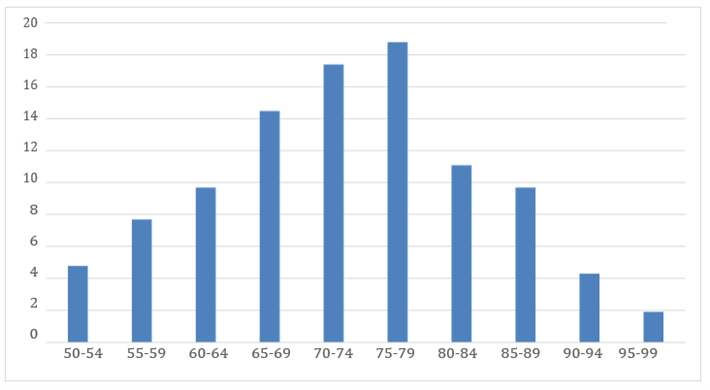
Figure 1: Age group distribution (N=207)
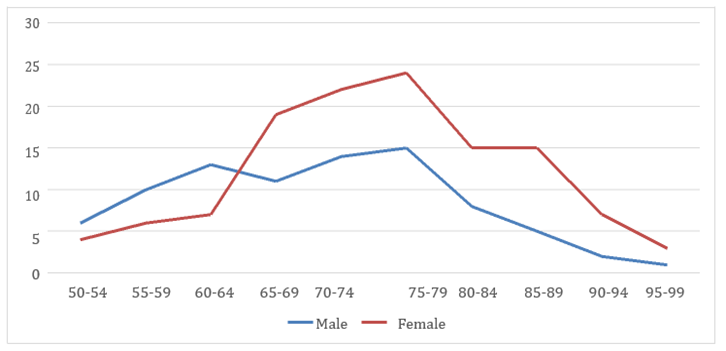
Figure 2: Age group distribution by number within each gender
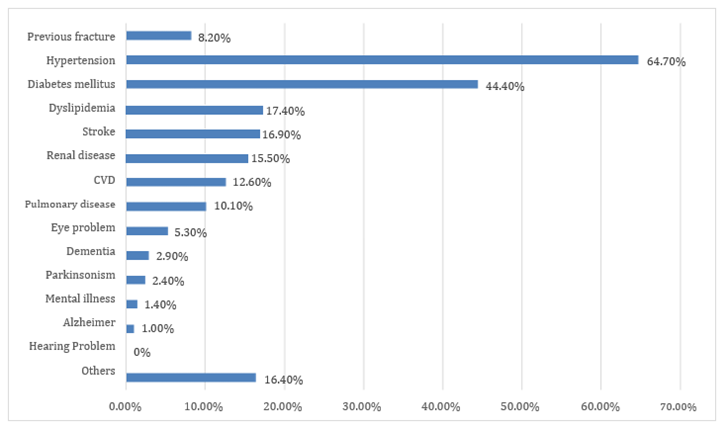
Figure 3: Patients with Co-morbids (N = 207)
Discussion
In this study, the majority of patients who sustained fragility fractures were female (58.9 %). According to the International Osteoporosis Foundation (IOF), about 61 % of osteoporotic fractures occur in women with a female-to-male ratio of 1.6 [1]. This is due to the rapid decrease in bone density occurring after menopausal and leads to osteoporosis [7].
The predominant age group for hip fracture in this study was with a mean (SD) age of 73.0 (10.7) years. The average life expectancy of Malaysians has increased from 73.3 years in the year 2009 to 75.0 in the year 2016 [8]. Fracture risk increase with each fragility fracture and aging. Studies of hip fracture by Lee JK et al and Isnoni I have reported that Chinese is the most affected ethnic group followed by Malay and Indian [9,10]. This correlates with our data and similar trends were seen in vertebrae and wrist fracture with Chinese predominantly affected. According to the National Population Census, in the year 2016, the majority of our population are Malay (68.6 %) followed by Chinese (23.4 %), Indian (7.0 %), and other ethnic (1.0 %).
Osteoporosis and many chronic diseases are associated with aging. The risk of falling increases with the presence of relevant chronic diseases, such as stroke, arthritis, depression, and diabetes. The chronic diseases that contribute to the risk of recurrent falls after the first are heart attack, angina, stroke, asthma, COPD, CKD, arthritis, depression, and diabetes [11]. In our present data, diabetes (44.4 %) is the second most common comorbid among fragility fracture patients. While the history of the previous stroke (16.9 %) and cardiovascular disease (12.6 %) are the 4th and 6th most common comorbid among patients. Although there is no data suggesting hypertension and dyslipidemia as risk factors of fall, these two are major risk factors to develop cardiovascular disease and cerebrovascular disease, indirectly increase the risk of future fall. Hypertension (64.7 %) and dyslipidemia (17.4 %) are the first and third most common comorbid among our data. The majority of our patients are at risk of falls and recurrent falls.
Guidelines from the National Osteoporosis Foundation (NOF) in 2014 recommended that adults who sustained a fracture above the age of 50 should have BMD [12]. In our study only about 13 % of patients with fragility fracture have BMD. A review of international studies reported only 1 % to 32 % of patients had their bone mineral density scans [13]. Another similar study by Kung et al that looks at post-menopausal women in Asian countries who had fragility fracture reported that only 28.2 % of them had BMD measurements [6]. A study by Angthong et al in Thailand also reported that only 38.2 % of patients underwent BMD testing [14]. BMD testing is important in diagnosing osteoporosis and predicting the risk of getting fractures in the future. In our study, the rate of BMD testing among patients was also low and this can be contributed due to a lack of general awareness. A study by Zaris et al has revealed the awareness and knowledge of the public regarding osteoporosis are low, despite age, gender, and level of education [15]. This might be observed among doctors for not correlating fragility fracture with osteoporosis and reducing the rate of BMD testing.
Advise of adequate intake of calcium and vitamin D daily should also be given to reduce the risk of sustaining a fracture in the future and this can be achieved by increasing their dietary intake or by giving supplements to the patients. Just over half of the patients were prescribed calcium and vitamin D in our study, in comparison with Gian Gregorio et al study which reported that only 2 % to 62 % of the patients in 10 Western countries were prescribed similar supplements [13] Thus, it can be said that our survey results are comparable to western countries with advanced medical care.
Many studies have shown, only about 20 % of osteoporotic fracture patients receive an assessment and treatment for osteoporosis [2]. This corresponds to our finding where only 19.3 % of patients were treated with anti-osteoporotic medication. The rate of calcium and vitamin D prescription was more than double compared with anti-osteoporotic treatment. One of the contributing factors is the price difference between the calcium and vitamin D supplements with anti-osteoporotic medications. In our study, over 70 percent of patients care at the age of retiring or non-working, leading to low affordability of osteoporosis treatment among patients. There are other possible contributing factors to low osteoporosis treatment rates, such as low awareness of osteoporosis and the belief that treatments are generally not worth their risk [15].
A multidisciplinary team approach has been recommended to manage patients with a fragility fracture and improve osteoporosis management thus preventing secondary fracture. International Osteoporosis Foundation has introduced a worldwide program ‘Capture the fracture’ where the hospital can implement Fracture Liaison Service (FLS) to tackle this problem. Bogoch et al. also argued that the role of orthopedic surgeons is not limited to only treating the patients with a fragility fracture, but they should also ensure that actions are being done to prevent subsequent fractures [16].
Conclusion
The persistent Osteoporosis care gap still exists for people suffering from fragility fractures. An increase in awareness among the doctors and improvement in the management of osteoporosis need to be emphasized to reduce secondary fractures which can lead to further morbidity and mortality in patients. One of the ways to improve this is to set up Fracture Liaison Service in our hospital setting as recommended by International Osteoporosis Foundation.
References
- Johnell O, Kanis JA (2006) An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int 17(12): 1726–1733.
- Papaioannou A, Giangregorio L, Kvern B, Boulos P, Ioannidis G, et al. (2004) The osteoporosis care gap in Canada. BMC Musculoskelet Disord. 5: 11.
- Dimitriou R, Calori G, Giannoudis P (2012) Improving patients’ outcomes after osteoporotic fractures. International Journal of Clinical Rheumatology. 7(1): 109-124.
- Hamdy RC, Baim S, Broy SB, Lewiecki EM, Morgan SL, et al. (2010) Algorithm for the management of osteoporosis. South Medl J. 103(10): 1009- 1015.
- Rabenda V, Vanoverloop J, Fabri V, Mertens R, Sumkay F, et al. (2008) Low incidence of anti-osteoporosis treatment after hip fracture. J Bone Joint Surg Am. 90 (10): 2142-2148.
- Kung AW, Fan T, Xu L, Xia WB, Park IH, et al. (2013) Factors influencing diagnosis and treatment of osteoporosis after a fragility fracture among postmenopausal women in Asian countries: a retrospective study. BMC Womens Health, 13: 7.
- Stavros CM (2010) From Estrogen-Centric to Aging and Oxidative Stress: A Revised Perspective of the Pathogenesis of Osteoporosis. Endocr Rev. 31(3): 266–300.
- Malaysian population statistic. Department of Statistic, Malaysia. 2016.
- Lee JK, Amir S MKHR (2007) The incidence of hip fracture in Malaysians above 50 years of age: variation in different ethnic groups. J Rheumatol. 10(4): 300–305.
- Isnoni I, Adam BM, Murallitharam M, Tajuddin A, Jaya Purany SP, et al. (2012) Pre-Injury Demographic Patterns of Patients Sustaining Hip Fractures in Malaysia. Malays Orthop J. 6(SupplA): 11–15.
- Yoshita P, Patricia WS, Scott MR (2017) Chronic Health Conditions as a Risk Factor for Falls among the Community-Dwelling US Older Adults: A Zero-Inflated Regression Modeling Approach. BioMed Research International. 2017: 5146378, 1-9.
- Cosman F, de Beur SJ, LeBoff MS, Lewiecki EM, Tanner B, et al. (2014) Clinician’s Guide to Prevention and Treatment of Osteoporosis. Washington, DC: National Osteoporosis Foundation. 25(10): 2359-81.
- Giangregorio L, Papaioannou A, Cranney A, Zyta ruk N, Adachi JD (2006) Fragility Fractures and the Osteoporosis Care Gap: An International Phenomenon. Seminars in Arthritis Rheum. 35(5): 293-305.
- Angthong C, Rodjanawijitkul S, Samart S, Angthong W (2013) Prevalence of bone mineral density testing and osteoporosis management following low- and high-energy fractures. Acta Orthop Traumatol Turc. 47(5): 318-322.
- Zaris SNABSM, Ahmad MSB, Mohamed SZB, Shuid AN, Naina MI, et al. (2016) Knowledge and awareness regarding osteoporosis among multi ethnic people attending the orthopaedic clinic at universiti kebangsaan malaysia medical centre. Malaysian Journal of Public Health Medicine. 16(3): 166-175.
- Bogoch E, Elliot-Gibson V, Beaton DE, Jamal SA, Josse RG, et al. (2006) Effective Initiation of Osteoporosis Diagnosis and Treatment for Patients with a Fragility Fracture in an Orthopaedic Environment. The Journal of Bone and Joint Surgery (American). 88(1): 25-34.



