Salma Mrichi1*, Mustapha Hemama2, Nizare El Fatemi2, Moulay Rachid El Maaqili2
1Department of Neurosurgery, Hôpital des spécialités, Mohamed V University of Rabat, Morocco
2Department of Neurosurgery, Ibn Sina Hospital, Mohamed V University of Rabat, Morocco
*Corresponding Author: Salma Mrichi, Department of Neurosurgery, Hôpital des spécialités, Mohamed V University of Rabat, Morocco
Abstract
Introduction: Ossification of the ligamentum flavum is a rare cause of thoracic myelopathy. It is a widely described pathology in eastern Asia and mainly in Japan. The exact pathophysiology has not been elucidated yet.
Case Description: A 28-year-old previously healthy male presented with progressive thoracic cord compression with a 3/5 paraparesis, urinary incontinence, and a mild functional disability. Blood reports showed no abnormalities. Computed tomography and magnetic resonance imaging showed a ligamentum flavum ossification at T1 and T2 levels with an intramedullary hyper signal T1-T3. A decompressive laminectomy with flavectomy was performed. At hospital discharge, the patient remained with paraparesis and urinary incontinence. At 3 months, he has a 4/5 paraparesis, without any sphincter or sensory alterations.
Conclusions: Symptomatic thoracic ossification of the ligamentum flavum is a rare pathology. This case adds to the previously reported cases of the occurrence of the disease in different populations.
Keywords: Ligamentum flavum ossification, thoracic cord compression, myelopathy
Introduction
The abnormal ossification of spinal ligaments is a well-known cause of myelopathy in East Asian populations, with ossification of the ligamentum flavum (OLF) and the posterior longitudinal ligament being the most prevalent.
Ossification of the ligamentum flavum was discovered by Polgar through a lateral X-ray film and further described by Yamaguchi and Isuruni [1], and it’s characterized by the growth and replacement of the ligamentum flavum with mature, lamellar bone.
Case Report
This is a case of a 28-year-old male who’s previously healthy with no history of prior trauma. He suffered from backache for 3 years without consulting. He complained of progressive gait disturbance for 9 months leading to walking incapacity as well as urinary incontinence at the time of admission to our department. On clinical examination, we found spastic paraparesis, hyperreflexia in both lower limbs, and a posterior cord syndrome with impairments of proprioceptive and vibration sense. The rectal sphincter was preserved. Therefore, the patient clinical condition corresponds to a 4 rating according to the modified scale of the Japanese Orthopedics Association (mJOA) [2].
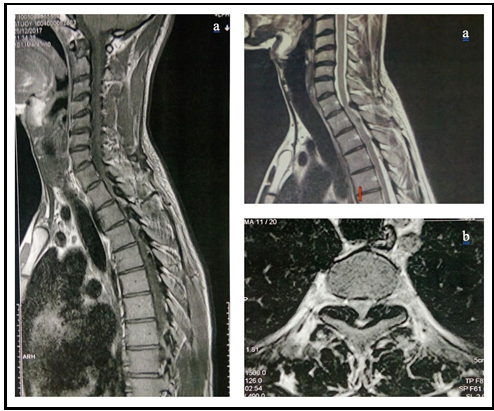
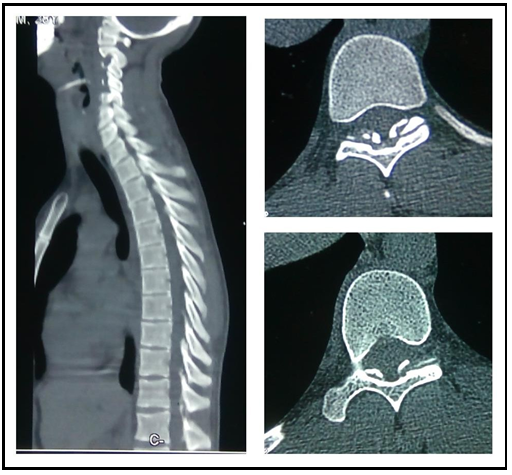
The T2-weighted sequence of MRI sagittal images showed a hypointense signal in the posterior portion of the vertebral canal on T1 and T2 levels (Figure 1a). Axial views showed spinal cord compression, especially on the T1 level (Figure 1b). We also observed an intramedullary hyper signal extending from T1 to T3. CT-Scan confirmed ligamentum flavum ossification, as well as the spinal canal stenosis, increased on the T1-T2 segment (Figure 2). We conclude to a spinal cord compression due to ossification of ligamentum flavum in the thoracic region.
Figure 1 a. T2-weighted sequence of MRI sagittal images showing hypointense signal in the posterior portion of the vertebral canal of T1. b. Axial views demonstrating spinal cord compression on the T1-T2 segment
Figure 2 CT-Scan confirming the ligamentum flavum ossification and spinal canal stenosis increased on T1-T2 level.
We completed the investigation by running blood tests. All serum levels of calcium, Vit D, alkaline phosphatase, uric acid, glucose, and parathyroid hormone were within the normal range.
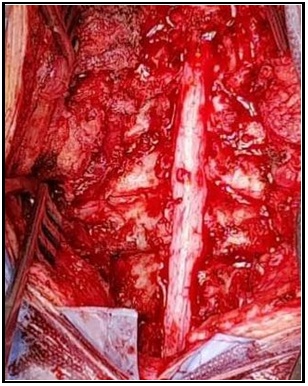
Posterior spinal decompression of the T1-T3 segment was proposed to the patient. Once the laminectomy was performed, we found a hardened ligamentum flavum and very adhered to the dura mater as expected. With careful dissection, we managed to resect the ossified ligamentum flavum on three levels without injuring the dura mater (Figure 3).
Figure 3 Three level laminectomy. Intact Dural sac after resection of ligamentum flavum shown here.
In immediate post-operative follow-up, we didn’t observe any worsening or improvement of his neurological status. His mJOA scale remained the same. Early rehabilitation is mandatory in such cases and corresponds perfectly with the patient's needs.
At the 3-month follow-up, the patient had significantly improved his neurological status, which included motor and sphincter functions. his mJOA score had risen to 7. he will pursue rehabilitation measures and will be evaluated again in 3 months.
Discussion
The ligamentum flavum is the ligament that connects the laminae of adjacent vertebrae from C2 to S1. It is known to be elastic but over time there can be a loss of strength and elasticity causing it to thicken therefore it can lead to spinal stenosis. We came across two potential theories behind the development of OLF: intrinsic factors like genetic and dietary factors [3] and extrinsic factors influencing the biomechanical changes. Chemical mechanisms leading to the OLF have been studied by numerous authors [4]. However, the pathophysiology behind it remains unclear.
Takafumi Yayama et al [5] published a paper in 2007 about the histopathology of OLF. They believed that when the tensile force increases, BMP-2, TGF-beta, and SOX are elevated in the ligamentum flavum. Then, the fibroblasts become differentiated into chondroblasts and osteoblasts, and finally, ossification of the ligament develops. Two events must coincide for the disease to emerge: the hyperplasia of the ligament and its further ossification [6].
Ossification of ligamentum flavum is encountered frequently in the thoracic region [7,8,9]. Toledo et al [10] believed that hyperkyphosis in the thoracic spine is commonly associated with mechanical stress, which makes ligaments in this region more prone to ossification [10]. OLF is commonly associated with other diseases. The following are some of the pathologies we found in the literature that can engender ligament hyperplasia and perhaps OLF: hypoparathyroidism, Paget’s disease, diabetes mellitus type 1 and 2, hyperthyroidism, hemochromatosis, fluorosis, hereditary vitamin D-resistant rickets, and diffuse idiopathic skeletal hyperostosis.
The clinical presentation consists of slowly progressive myelopathy characterized by a posterior cord syndrome given that the compression begins from the posterior side [3]. Over time, as the process of ossification progresses, spastic paraparesis develops due to compression of lateral corticospinal tracts.
MRI and CT scans are necessary for OLF diagnosis. CT provides key information on the topography and extent of OLF with a fine analysis of the spine that MRI barely pictures. This information is the cornerstone of proper surgical planning. When it comes to MRI, the focus is on evaluating the relationship between OLF and the structures within the spinal canal, especially the dura mater, as well as looking for signs of spinal cord injury due to compressive phenomena.
Sato [11] classified this disorder according to its progression:
- Lateral type which means ossification of only the capsular portion of the ligamentum flavum.
- Extended type which means extended ossification of the interlaminar portion.
- Enlarged type which means anteromedial thickening and enlargement of ossification.
- Fused type which means fusion of the bilateral ossified masses at the midline.
- Tuberous type which means anterior growth of the fused mass of ossification.
The management strategy depends on the involved level (s) and whether or not there is multi-level involvement. For most cases, laminectomy is the gold standard procedure as it provides a wide decompression of the spinal canal. Let’s keep in mind the potential kyphosis one could encounter after performing a multiple-level laminectomy. One may switch to laminoplasty with the drilling of the ossified ligamentum flavum instead of classic laminectomy as an acceptable solution whenever multiple levels are involved.
Among the reported factors of poor prognosis, we found when reviewing the literature [12,13], old age, severe preoperative symptoms, and their long duration before surgery, rapid onset of symptoms, dural adhesion, and ossification, intramedullary high signal intensity same as our patient, the severity of morphological classification and multi-level injury.
Patients with OLF should be followed up closely with frequent radiological examinations as the disease will continue to progress and eventually affect further spinal levels.
Conclusion
Ossification of ligamentum flavum is a rare cause of slowly progressive thoracic myelopathy one should be aware of to prevent irreversible symptoms. Radiographic findings are pathognomonic.
Surgical decompression through laminotomy or laminoplasty is the best surgical option to the best of our knowledge.
Credit Authorship Contribution Statement
Salma Mrichi: Conceptualization, data collection, paper preparation, writing;
Mustapha Hemama: Conceptualization, Nizare El Fatemi: study design, validation, review & editing. Moulay Rachid El Maaqili: Validation, review & editing.
Conflicts of Interest: The authors declare not having any conflict of interest.
Funding Sources: The authors declare not to have any funding sources for performing the research.
References
- H. Yamaguchi, S. Tamagake, et S. Fujita, « A case of ossification of the ligamentum flavum with spinal cord tumor symptoms », Seikeigeka, vol. 11, no 3, p. 951, 1960.
- Benzel EC, Lancon J, Kesterson L, Hadden T (1991) Cervical laminectomy and dentate ligament section for cervical spondylotic myelopathy. J. Spinal Disord. 4(3): 286‑295.
- Ahn DK, Lee S, Moon SH, Boo KH, Chang BK, et al. (2014) Ossification of the Ligamentum Flavum. Asian Spine J. 8(1): 89‑96.
- Li H, Jiang LS, Dai LY (2007) Hormones and growth factors in the pathogenesis of spinal ligament ossification. Eur Spine J. Off. Publ. Eur. Spine Soc. Eur. Spinal Deform. Soc. Eur. Sect. Cerv. Spine Res. Soc. 16(8): 1075‑1084.
- Yayama T, Uchida K, Kobayashi S, Kokubo Y, Sato R, et al. (2007) Thoracic ossification of the human ligamentum flavum: histopathological and immunohistochemical findings around the ossified lesion. J. Neurosurg. Spine. 7(2): 184‑193.
- Okada K, Oka S, Tohge K, Ono K, Yonenobu K, et al. (1991) Thoracic myelopathy caused by ossification of the ligamentum flavum. Clinicopathologic study and surgical treatment. Spine. 16(3): 280‑287.
- Guo JJ, Luk KD, Karppinen J, Yang H, Cheung KM (2010) Prevalence, distribution, and morphology of ossification of the ligamentum flavum: a population study of one thousand seven hundred thirty-six magnetic resonance imaging scans. Spine. 35(1): 51‑56.
- Lang N, Yuan HS, Wang HL, Liao J, Li M, et al. (2013) Epidemiological survey of ossification of the ligamentum flavum in thoracic spine: CT imaging observation of 993 cases. Eur. Spine J. 22(4): 857‑862.
- Fong SY, Wong HK (2004) Thoracic myelopathy secondary to ligamentum flavum ossification. Ann. Acad. Med. Singapore. 33(3): 340‑346.
- Toledo JA, Isseldyk FV, Re M, Garrote M (2013) Ossification of the ligamentum flavum as cause of thoracic cord compression: Case report of a Latin American man and review of the literature. Surg. Neurol. Int. 4: 119.
- Sato T, Kokubun S, Tanaka Y, Ishii Y (1998) Thoracic myelopathy in the Japanese: epidemiological and clinical observations on the cases in Miyagi Prefecture. Tohoku J. Exp. Med. 184(1): 1‑11.
- Nishiura I, Isozumi T, Nishihara K, Handa H, Koyama T (1999) Surgical approach to ossification of the thoracic yellow ligament », Surg. Neurol. 51(4): 368‑372.
- Trivedi P, Behari S, Paul L, Banerji D, Jain VK, et al. (2001) Thoracic myelopathy secondary to ossified ligamentum flavum », Acta Neurochir. (Wien). 143(8): 775‑782.