Ismaël Daoudi1*, Ayoub Drissi-Bakhkhat2, Farouk Dargai3, Soraya Daoudi4
1Orthopedic surgery resident, Centre Hospitalier Universitaire de la Reunion, CHU Felix Guyon (Saint Denis) Allée des topazes CS 11 021 Saint- Denis 97400, Réunion
2Internal medicine resident, Centre Hospitalier Universitaire de la Reunion, CHU Felix Guyon (Saint Denis) Allée des topazes CS 11 021 Saint- Denis 97400, Réunion
3orthopedic surgeon, Centre Hospitalier Universitaire de la Reunion, CHU Felix Guyon (Saint Denis) Allée des topazes CS 11 021 Saint-Denis 97400, Réunion
4Pediatrician, Centre Hospitalier Universitaire de la Reunion, CHU Felix Guyon (Saint Denis) Allée des topazes CS 11 021 Saint-Denis 97400, Réunion
*Corresponding Author: Ismaël Daoudi, Orthopedic surgery resident, Centre Hospitalier Universitaire de la Reunion, CHU Felix Guyon (Saint Denis) Allée des topazes CS 11 021 Saint-Denis 97400, Réunion
Introduction
Tuberculosis is a common infectious disease worldwide. Abdominal tuberculosis is the sixth most common site of extra-pulmonary involvement and can affect any part of the digestive system with the most frequent site being the ileocecal region [1]. Its prevalence is around 1 % when associated with mild pulmonary localization [2]. The main differential diagnosis is Crohn’s Disease. Besides, most importantly, it is essential to differentiate one diagnosis from another as the treatments for hypothetical chronic inflammatory bowel diseases could actually lead to worsening the prognosis of an ignored tuberculosis. Diagnosis of digestive tuberculosis includes clinical and biological elements, imaging & endoscopic screening, but confirmation is always given by pathology, with the highlighting of Mycobacterium.
Case description
Our patient was a 40 years old male with a medical history of chronic alcohol abuse. He consulted his gastroenterologist in August 17’ for chronic abdominal pain, leading to endoscopic findings as colonoscopy showed cecal and colic ulcerated lesions, EGD being normal. Biopsies pointed out the presence of epithelioid granulomas without caseous necrosis associated with plasmocytary infiltration. MR enterography showed terminal small bowel lesions. First-line treatment for the suspected IBD by Budesonide is launched, quickly replaced by prednisone as the patient kept suffering from massive weight loss and abdominal pain on January 18’.
A few weeks later, the patient consults for alteration of general state with important weight loss up to 22 % in 5 months, diffuse abdominal pain with rectal bleeding, but no history of fever, aphthosis, diarrhea with blood, and mucus nor any extra digestive symptom. Blood tests only highlighted elevated C-Reactive Protein, without abnormality of blood count. Abdominal CT objectified ileocecal lesions with peritoneal effusion but without any apparent fistula.
A rectosigmoidoscopy explained the rectal bleeding as having been caused by internal hemorrhoids. Pre-treatment check-up is launched before anti-TNF-α is started: all results are favorable except IGRAs, local conditions involving a 10 days delay. However, the disease outbreak is brutal, our patient has quickly been treated with prednisone 20mg per day, antibiotics are associated (ceftriaxone and metronidazole) for a supposed unseen fistula on CT, and Infliximab is started as long as parenteral nutrition. After a 2 weeks stay at the hospital, abdominal pain is relieved and nutritional assessment is satisfactory, the patient is allowed to reach home, with oral corticotherapy.
1 week later, consultation for bilious vomiting and fever. Abdominal CT is performed showing signs of disease outbreak and suspicion of terminal small bowel fistula. Corticotherapy has majored to 40mg a day and the second line of Infliximab is administrated with a doubled dose.
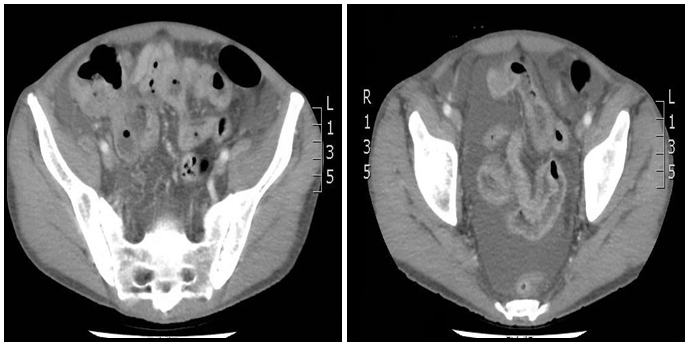
Figure 1a et 1b: Abdominal CT Scan showing abundant intra peritoneal effusion associated with signs of diffuse ileitis with suspected small bowel fistula.
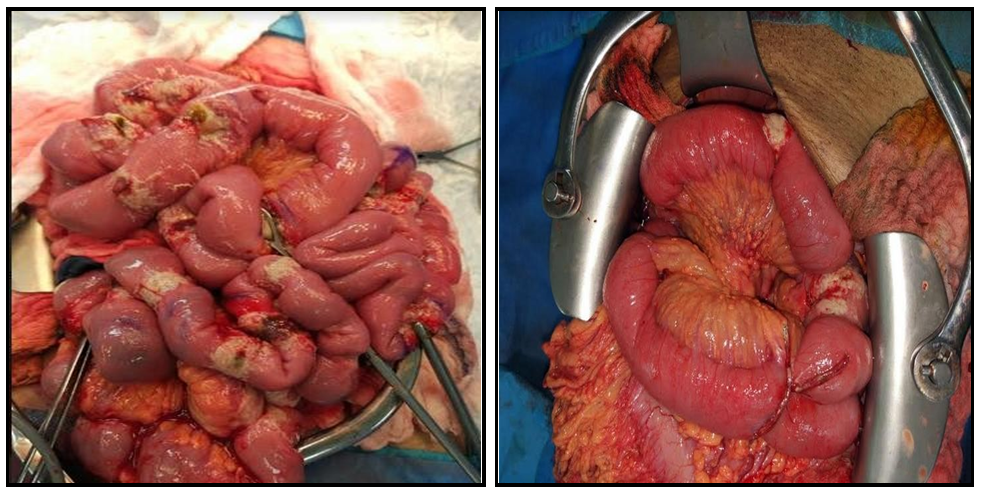
Digestive hemorrhages appeared 5 days later leading to repeated red cells transfusions and an endoscopic check-ups showed extension of the ulcerated lesions extended to the right colic angle associated with stenosis of the ileocecal valve. Active bleeding was treated surgically and showed perforated lesions concerning the entire small bowel, with « grains of rice »-like nodules and bowel necrosis, seeming untypical of the initial diagnosis of Crohn’s Disease.
Figure 2a et 2b: Surgical aspect showing multiple perforated and ulcerated small bowel lesions associated to tuberculous granulation tissue with rice bodies in the mesentery. Features rather not consistant with a Crohn’s Disease as there is no typical mesenteric liposclerosis.
Regarding the highly suspected diagnosis of Disseminated Tuberculosis, combination therapy is started (rifampicin, isoniazid, and ethambutol) Pathology reveals multiple bacillary lesions, perforative or pre perforative in all digestive samples analyzed.
Biological material from the surgery was positive for bacterial peritonitis caused by Enterobacter cloacae, Staphylocoque haemolyticus & Stenotrophomonas maltophilia.
Bronchial aspiration in the intensive care unit shows mycobacterium.
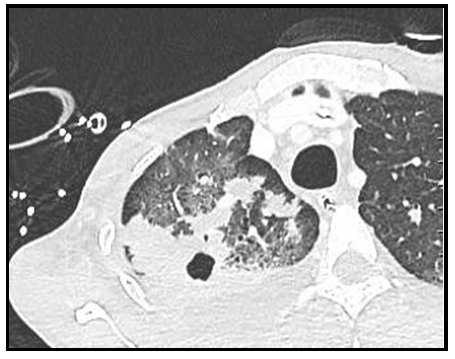
Thoracic CT gives a typical aspect of bilateral apical lesions evocative of sévère active tuberculosis.
Inspection of the first chest X-Ray retrospectively contains compatible elements of pulmonary lesions and IGRAs turned out to be positive just before the patient left the hospital at his first stay.
3 days later, surgeons performed a second look surgery and completed segmental small bowel resections with manual anastomosis, right colectomy, samples showing perforated caseous necrosis.
Surgical follow-up was marked by cardiogenic and hypovolemic shock, multifactorial cardiac dysfunction due to tubercular myocarditis, Refeeding syndrome, Macrophage-activation syndrome, long term parenteral nutrition, Critical illness neuromyopathy worsened by the nutritional state of the patient.
Figure 3a, 3b, 3c, 3d : The histological aspect of the lesions is identical in all analyzed intestinal samples. The lesions appear richly bacillary with a Ziehl-Neelsen stain. We can see wide ranges of caseous necrosis, the inflammatory reaction is dominated by a lymphocytic tissue but remains mostly macrophagic with an overload of cellular debris.
Figure 4 : Excavated lesion of 13 x 19 mm in the posterior segment of the upper right lobe, contiguous with a segmental bronchus. Infiltrated and condensed lesions prevailing in the upper right lobe, confluent, with air bronchogram. Bilateral pleural effusion.
Discussion
What makes these microscopic slides so particular are the big ranges of amorphous eosinophilic caseous necrosis surrounded with polymorphic inflammatory cells with a majority of neutrophils and macrophages associated with a thin granulomatous and epithelioid component. It is very likely that the double immunosuppression induced by corticoids and infliximab received by our patient was responsible for the particular aspect shown by the first slides, which led us to the diagnosis of Crohn’s Disease. Interestingly, when it comes to immunocompetent patients suspected of digestive tuberculosis, Ziehl-Neelsen stain is almost always negative and most of the time slides mostly show inflammatory aspects associated with the granulomatous reaction.
In this case, the decision of immunosuppression by anti-TNF alpha was made by the presence of a negative Mantoux test while the results of the IGRA were still unavailable. It is thus necessary to remind that there are numerous causes of wrongly negative Mantoux tests among which: [3]
A technical error (altered tuberculin, injection made too deep, late reading, and underestimated diameter of the induration);
The realization of the test during the pre-allergic phase of latent tuberculosis or a vaccination (less than 2 months after contamination or administration of the BCG);
The realization of the test during the evolution of disease responsible for tuberculin anergy such as a viral infection, a severe bacterial infection, a malignant hematological disease, immunosuppression, malnutrition, etc.
The reactivity to tuberculin is lowered within elderly people.
In this case, it is likely that the treatment by high-dose corticoids associated with severe malnutrition contributed to obtaining a negative Mantoux test.
The issue of making the difference between Crohn’s Disease and digestive tuberculosis is well known as these two are close in terms of histologic aspects and a few elements allow to differentiate it firmly, i.e., caseous necrosis & identification of mycobacterium on the slides. The macroscopic aspect of the lesions (ulcerous and hemorrhagic) usually guides the pathologist towards a diagnosis of chronic inflammatory disease but can be a source of error in particular when the patient presents no sign of associated lung disease, as isolated digestive tuberculosis is exceptional.
As for us, we are still wondering whether it is a Crohn’s Disease-associated digestive tuberculosis or an actual isolated digestive tuberculosis with an altered aspect caused by immunosuppression.
|
Author |
Year of publication |
Age |
History |
Method of discovery |
Treatment |
Topography |
|
Lwin S [3] |
2017 |
31 |
pregnancy |
abdominal pain/ Diarrhea/loss of weight |
right hemicolectomy |
Jejunum |
|
Ngonge Al [4] |
2017 |
31 |
VIH |
Progressive abdominal distention/ drenching night sweat/ generalized fatigue without fever |
Resection of the necrotic jejunal segment with a primary end-to- end anastomosis |
Caecum |
|
Swain SK[5] |
2017 |
57 |
None |
pain in the upper abdomen/loss of appetite and weight loss of 4 kg in 4 months. |
elective surgery |
Colon transverse |
|
Masood I [6] |
2015 |
25 |
None |
progressively worsening abdominal pain/ fatigue and weight loss for the past 8 months. |
Perforations were primarily closed by suture while the perforations at the terminal ileum were resected, and two ends were brought out as double-barreled ostomy |
pan-enteric perforation |
|
Kok-Hong Chan D |
2015 |
68 |
sarcoidosis / Immunosuppress ion |
abdominal pain |
A segment of the small bowel containing the perforation was resected |
Ileum |
|
Wu YF [7] |
2015 |
42 |
previously mistreated with Crohn’s disease. |
recurrent abdominal pain and weight loss (15 kg) in 2 years |
emergency resection of the diseased small bowel and temporary ileostomy, followed by 6-month standard treatment for miliary tuberculosis |
terminal ileum |
|
Tahmasebi S [8] |
2013 |
62 |
VIH |
anorexia, 12 pounds weight loss intermittent fever |
repaired both bowel perforations |
Jejunum and ileum |
|
Sanjay Gupta [9] |
2013 |
30 |
None |
fever/ generalized abdominal pain for one day, signs of peritonitis |
the ileal perforation was freshened along the margins and closed primarily using interrupted sutures |
terminal ileum |
|
Devendra K Jain [10] |
2010 |
39 |
chronic alcoholic |
right lower quadrant abdominal pain and low-grade fever of 2 days duration |
right hemicolectomy with ileostomy and the transverse colonic mucous fistula was done |
caecum |
Conclusion
We added to the actually available literature the case of a 40-year-old patient presenting disseminated digestive tuberculosis that appeared or worsened by Infliximab, resulting in polymicrobial peritonitis due to multiple perforated digestive necroses, with multiple intestine resections, which is still uncertain for an associated Crohn’s Disease.
Key clinical message:
It is essential to differentiate abdominal tuberculosis and Crohn's disease before introducing treatment with immunosuppressants which the consequences can be serious or even fatal in the event of an infectious disease like tuberculosis.
References
- Sharma M, Bhatia V (2004) Abdominal tuberculosis. Indian J Med Res. 129(4): 305–15.
- Donoghue HD, Holton J (2009) Intestinal tuberculosis. Curr Opin Infect Dis. 22(5): 490-6
- Revue des maladies respiratoires [Vol. 20 - N° 6-C2 - p. 733-0] : L’intradermo-réaction à la tuberculine (IDR) ou test à la tuberculine. 2003
- Lwin S, Jing NLL, Suharjono H, Kipli MB, Moe Nwe T, et al. (2017) Caecal Perforation from Primary Intestinal Tuberculosis in Pregnancy. Case Rep Gastrointest Med. 2017: 2173724.
- Ngonge AL, Ekaney DSM, Sama CB, Musonge-Effoe J, Effoe VS, et al. (2017) Multiple jejunal perforation secondary to intestinal tuberculosis infection: a case report. Pan Afr Med J. 27: 78.
- Swain SK, Zirpe D, Das S, Balachandar TG, Reddy PK (2017) Parietal Wall Abscess Perforating to Transverse Colon: A Rare Presentation. J Clin Diagn Res. 11(5): PD10-PD11.
- Masood I, Majid Z, Rafiq A, Rind W, Zia A, et al. (2015) Multiple, Pan-Enteric Perforation Secondary to Intestinal Tuberculosis. Case Rep Surg. 2015: 318678.
- Kok-Hong Chan D, Lee KC (2015) Perforated Intestinal Tuberculosis in a Non-AIDS Immunocompromised Patient. Am J Case Rep. 16: 719-22.
- Wu YF, Ho CM, Yuan CT, Chen CN (2015) Intestinal tuberculosis previously mistreated as Crohn's disease and complicated with perforation: a case report and literature review. Springer plus. 4: 326.
- Tahmasebi S, Moslemi S, Tahamtan M, Taheri L, Davarpanah MA (2013) Asymptomatic Tuberculosis-Induced Ileal Perforation in an HIV- Infected Individual; A Case Report. Bull Emerg Trauma. 1(4): 182-5.
- Gupta S, Jayant M, Kaushik R (2013) Free tubercular perforation of the ileum. World J Emerg Med. 4(3): 235-6.
- Jain DK, Aggarwal G, Lubana PS, Moses S, Joshi N (2010) Primary tubercular caecal perforation: a rare clinical entity. BMC Surg. 10: 12.