Héctor Ricardo Galvan Garcia MD1*, Gabriel Esteban Salerni MD2, María Marcela Moran Ybarra MD3, Teresa Berenice MD4
1Hospital Dermatológico, Dermoquirurgica. Guadalajara, Jalisco, México.
2National University of Rosario, Rosario, Argentina. Centenario Provincial Hospital of Rosario, Rosario, Argentina
3Hospital de Especialidades Dr Antonio Fraga Mouret Centro Médico Nacional IMSS La Raza
4Hospital Regional ISSSTE León
*Corresponding Author: Héctor Ricardo Galvan Garcia MD, Hospital Dermatológico, Dermoquirurgica. Guadalajara, Jalisco, México.
Abstract
Background: Thousands of people in latin america suffer from melasma:
Aims: Dermatoscopy is an effective method for melasma diagnosis.
Patients and Methods: 40 patients with diagnosis of melasma were included and examined with a dermatoscope Dermlite L5 and dermatoscope Fotofinder Medicam 800HD.
Results: We found a total of 40 patients with diagnosis of melasma. One patient with vascular melasma, seventeen pigmentary melasma and 22 mixed melasma.
Conclusion: Our dermoscopic patterns were similar to asian patients compared to the melasma patients in Latin America.
Introduction
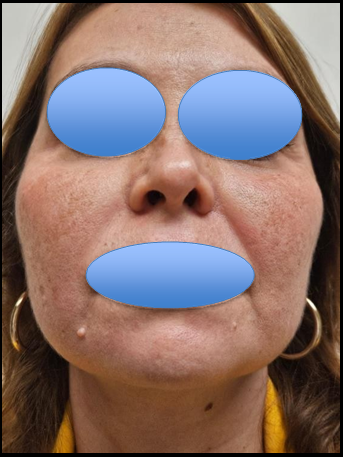
Melasma, a common dermatological condition characterized by the presence of hyperpigmented patches and macules, typically manifests on the facial skin. This condition predominantly impacts adult females, particularly those with Fitzpatrick skin phototypes III to V. [1] (figure 1).
Figure 1: Melasma Skin Type 4.
Dermoscopy is a non-invasive, in-vivo technique that has traditionally been useful for the evaluation of suspicious skin lesions.
It can help identify lesions and differentiate melanocytic lesions from dysplastic lesions, melanomas, or non-melanoma skin cancers such as basal cell carcinoma or squamous cell carcinoma. [2] Furthermore, over the past several years, the use of dermoscopy has expanded to include utilization for diagnosis of dermatological disorders including inflammatory dermatosis, pigmentary dermatosis, infectious dermatosis, and disorders of the hair, scalp, and nails. As the utility of dermoscopy continues to expand, practitioners in almost all specialties should be familiar with this simple, non-invasive and high- yield diagnostic technique.
Dermoscopy can be used to determine the depth of melasma, to differentiate it from other conditions causing facial hyperpigmentation, to monitor treatment efficacy and to pick up early complications such as atrophy, telengiectasia and development exogenous ochronosis. [3]
Melasma is a common skin problem caused by brown to gray-brown patches on the face. Most people get it on their cheeks, chin, nose bridge, forehead, and above the upper lip. It is more common in women than men. (figure 2)
Figure 2: Melasma In Men.
Pregnancy is a common cause of melasma. It also affects woman taking oral contraceptives and hormones. [4,5,6,7]
The incidence rate of melasma in men is lower than that in women. The etiopathogenesis of melasma in men is considered to be similar to that in women, with the notable exception of the influence of estrogen [8]
The pathogenesis of melasma is highly complex with multiple pathologies occurring outside of the skin pigment cells. It includes photoaging, excessive melanogenesis, an increased number of mast cells, increased vascularization, and basement membrane damage. In addition, skin lesions related to melasma and their surrounding skin have nearly 300 genes differentially expressed from healthy skin.[9] According to the location of the skin lesions, they are generally divided into three types: I) The central facial type, in which the lesions are distributed on the forehead, (figure 3) cheek, upper lip, nose and chin, and this type is the most common; II) the cheek type, in which the lesions are distributed on the cheeks and nose (figure 5); and III) the mandibular type, in which the lesions are distributed on the area where the branches of the mandibular nerve (figure 5) are located. [10]
Figure 3: Melasma Central Facial.
Figure 4: Melasma Cheek.
Figure 5: melasma mandibular.
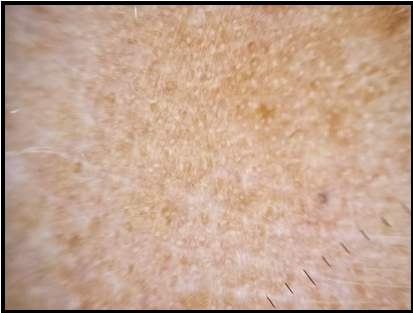
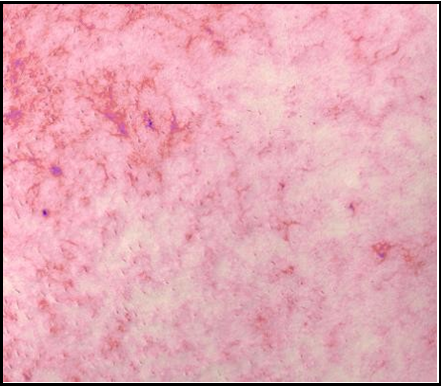
Dermoscopy is a non-invasive and in-vivo diagnostic tool, which visualises subtle clinical patterns of skin structures not visible to the unaided eyes. Dermatoscopy term was introduced in 1920 by German dermatologist Johann Saphier, but Goldman was the first person to use it for pigmentary lesions. The colour intensity of melanin and the regularity of the pigment network reveal the density and location of melanin. Melanin pigment appears as a dark brown colour with a well-defined network when located in stratum corneum. Whereas, it shows shades of light brown with an irregular network when located in lower layers of the epidermis and blue or bluish grey colour when located in the dermis.in 2009, Tamier,Carla and cols, they publish a study comparing Wood´s light and dermatoscopy in the diagnosis of melasma, classifyingit into three : pigmentary (figure 6), vascular (figure 7) and mixed (figure 8). [11]
Figure 6: melasma pigmentary.
Figure 7: melasma vascular.
Figure 8: Melasma Mix.
Dermoscopy can be used to determine the depth of melasma, to differentiate it from other conditions causing facial hyperpigmentation, to monitor treatment efficacy and to pick up early complications such as atrophy, telengiectasia and development exogenous ochronosis. In our study, we classified the melasma clinically and correlated with the dermoscopic findings. [12]
In addition, in clinical practice, dermoscopy are used in combination with histopathological analyses to divide melasma into the following types: I) Epidermal type: This type has a strong colour contrast under dermoscopy analysis found pigment deposition in the basement layer and the upper part of the basement layer II) Dermal type: In this type, the colour contrast between the lesions and the normal skin is not obvious under dermoscopy, and histopathological analysis revealed that there are melanophages around the upper and middle blood vessels of the dermis; III) Mixed type: The colour contrast of some parts of the same patient under dermoscopy is obvious, while that of other parts is not obvious, and histopathological analysis demonstrated that there are pigments in the epidermis and dermis [13]
Material and Methods
In this study, 40 patients from Mexico were included. They were randomly selected from consultations from august to december 2023, with a melasma diagnosis, the objective is to observe the dermoscopic pattern of each clinical type. The age range of the study group was between 37 to 70 years with 39 female participants and 1 male participant, 100% of the participants were with no medication and without cormobidities.
All patients were examined with a dermatoscope Dermlite L5 and dermatoscope Fotofinder Medicam 800HD., According to their clinical type, 22 were mixed, 17 pigmentary and 1 vascular. On topographical classification 13 presented central facial afectation, 34 in the malar region and 12 in the jaw region.
According to their dermoscopic classification 24 cases included the epidermis and 10 were mixed. The dermoscopic criteria included were the presentation of the brown background, pseudoreticular pigment network, globular pattern, dot pattern, arcuate pattern, visibles telangiectasias and, perifollicular pigmentation.
Results
Out of all of the 40 patients, only 1 presented vascular affection in the central facial region from the epidermic type, in dermatoscopy telangiectasias and perifollicular pigmentation were visible. (Table 1) 17 patients were of the clinical pigmentary type, from which 16 of them were predominantly affected in the malar region, 5 of them in the mandibular area and 2 in the central face, 12 of them encompassed the epidermis, 3 the dermis and 2 of them mixed. On dermatoscopy, 15 of them presented a brown background, 14 a pseudoreticular pigment network, 9 perifollicular pigment, 5 an arcuate pattern, 4 of them a dot pattern and 2 a globular pattern.
From the clinical mixed type, 18 out of 22 patients encompassed the malar region, 10 of them the central facial area and 7, the mandibular area. 11 Had affectations in the epidermis, 8 of them mixed and 3 in the dermis. On dermatoscopy telangiectasias were found in 19 of the cases, 17 with a brown background and pseudoreticular pigment network, in 14 of them perifollicular pigment was found, 4 with a dot and arcuate pattern and 3 with dot pattern. (Table 2 and 3)
Table 1: Number of Patients
|
Patients 40 total |
Vascular 1 |
Pigmentary 17 |
Mix 22 |
Table 2: Type of melasma
|
Vascular 1 |
Pigmentary 17 |
Mix 22 |
|
Terangiectasias 1 (100%)
Perifollicular Pigmentation 1 (100%) |
Brown Backgrond15(88%)
Pseudoreticular
Pigment Network 14(82%)
Perifolicular Pigment 9(52%)
Arcuate Pattern 5(29%)
Globular Pattern 2(11%) |
Telangiectasias 19(82%)
Brown
Backgrond 17(77%)
Perifolicular Pigment 14(63%)
Arcuate Pattern 4(18%)
Dote Pattern 3(13%) |
Table 3: Anatomical área of melasma
|
Vascular 1 |
Pigmentary 17 |
Mix 22 |
|
Central facial área 1 (100%) |
Malar area 10(58%) Mandibular área 5(27%) Central face area 2(11%) |
Malar área 18(81%) Mandibular área 2(9%) Central face area 2(9%) |
Conclusions
Our findings in Latin American melasma patients were similar from those described in Asian patients. The pigmentary and mixed type were more predominant as well as the dermoscopic patterns brown backgrond, pseudoreticular pigment network and perifolicular pigment.
References
- Vaneeta S, Amit P (2011) Melasma: A comprehensive update Part I. Journal of the American Academy of Dermatology. 65(4): 689- 97.
- Kaliyadan F (2016) The scope of the dermoscope. Indian Dermatol Online J. 7(5): 359-363.
- Bisalvadi L N, Joice M J, Kalasapura R R (2017) A clinico dermoscopic study of melasma in a tertiary care center. Pigment International. 4(2): 98 - 103.
- Sarkar R, Ghunawat S, Narang I, Verma S, Garg VK, et al. (2019) Role of broad-spectrum sunscreen alone in the improvement of melasma area severity index (MASI) and Melasma Quality of Life Index in melasma. J Cosmet Dermatol. 18(4): 1066-1073.
- Yeung H, Kahn B, Ly BC, Tangpricha V (2019) Dermatologic Conditions in Transgender Populations. Endocrinol Metab Clin North Am. 48(2): 429-440.
- Ching D, Amini E, Harvey NT, Wood BA, Mesbah Ardakani N (2019) Cutaneous tumoural melanosis: a presentation of complete regression of cutaneous melanoma. Pathology. 51(4): 399-404.
- Roberts WE, Henry M, Burgess C, Saedi N, Chilukuri S, et al. (2019) Laser Treatment of Skin of Color for Medical and Aesthetic Uses With a New 650-Microsecond Nd:YAG 1064nm Laser. J Drugs Dermatol. 18(4): s135-137.
- Sarkar R, Ailawadi P, Garg S (2018) Melasma in Men: A review of clinical, etiological, and management issues. J Clin Aesthet Dermatol. 11(2): 53–59.
- Piętowska Z, Nowicka D, Szepietowski JC (2022) Understanding Melasma-How Can Pharmacology and Cosmetology Procedures and Prevention Help to Achieve Optimal Treatment Results? A Narrative Review. Int. J. Environ. Res. Public Health. 19(19): 12084.
- Negbenebor NA, Heath CR, Usatine RP (2023) Melasma. J Fam Pract. 72(3): 133–137.
- Carla T, Fonseca R, Maria R, Pereira BC, Francisco, et al. (2009) Classificao do melasma pela dermatoscopia: estudio comparativo con lámpara de wood. Surgical and Cosmetic. 1(3): 115-119.
- Solanki V., Dongre A., Nayak C (2024) A clinico- epidemiological study of different dermoscopic patterns in hyperpigmented facial lesions in a tertiary care centre. Journal of Cutaneous and Aesthetic Surgery. 17(2): 112-123.
- Chen Y, Vellaichamy G, Schneider SL, Kong W, Liu Z (2024) Exposure factors in the occurrence and development of melasma (Review). Exp Ther Med. 27(4): 131.