Sailaja Nandennagari1, Ilhan Abdi1, Javairia Ayyub2, Pablo Schaerer3, Preethi Annam1, Reshma Annam4, Krupavaram Bethala5*
1Avalon University School of Medicine, Curaçao
2Caribbean Medical University School of Medicine, Curaçao
3Catholic University of Asunción
4Windsor University School of Medicine, St. Kitts
5KPJ Healthcare University College, Kuala Lumpur, Malaysia
*Corresponding Author: Krupavaram Bethala, KPJ Healthcare University College, Kuala Lumpur, Malaysia.
Abstract
Alcohol-induced liver cirrhosis in young adults aged between 25 to 35 years is very rare as cirrhosis needs to be achieved through a progression from fatty liver fibrosis to cirrhosis. It takes around 10 to 15 years to occur, meaning the patient should have started drinking in their teenage years, which is rare. Our case study presents a rare case of a 30-year-old female diagnosed with pancytopenia secondary to alcohol-induced liver cirrhosis. The purpose of this case study is to emphasize the effects of pancytopenia secondary to alcoholic liver disease on the wound-healing process of status post craniotomy for her fractured skull due to her recurrent falls.
Keywords: Cirrhosis, pancytopenia, alcohol, etc.
Introduction
Cirrhosis is considered to be the last stage of progressive hepatic fibrosis that is characterized by damage to the liver and irreversible damage to the formation of regenerative nodules. Once this occurs, liver cells can no longer replace or regenerate healthy tissue, which affects the liver's normal function. Cirrhosis has two stages, compensated and decompensated. Diagnosis involves clinical symptoms, labs, and imaging such as ultrasound (US). As mentioned above, many people are not aware of the severity of the disease as they are usually asymptomatic [1]. Although this is a disease of the late middle-aged male population, our case report represents a rare case with a decompensated stage of cirrhosis. A 30-year-old female with a social history of alcohol abuse develops alcoholic hepatitis, pancytopenia, hyponatremia, and liver cirrhosis with hepatic encephalopathy, among other complications, due to excessive alcohol intake. This paper focuses on the effects of a patient's pancytopenia on the wound-healing process secondary to alcoholic liver cirrhosis.
Alcoholic liver disease and Pancytopenia
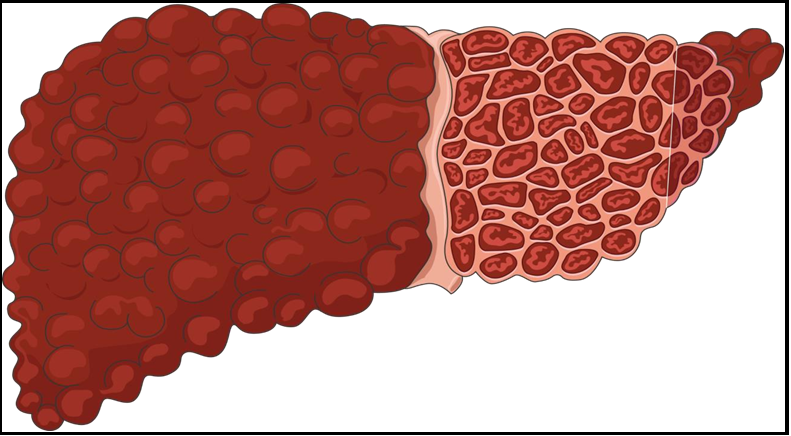
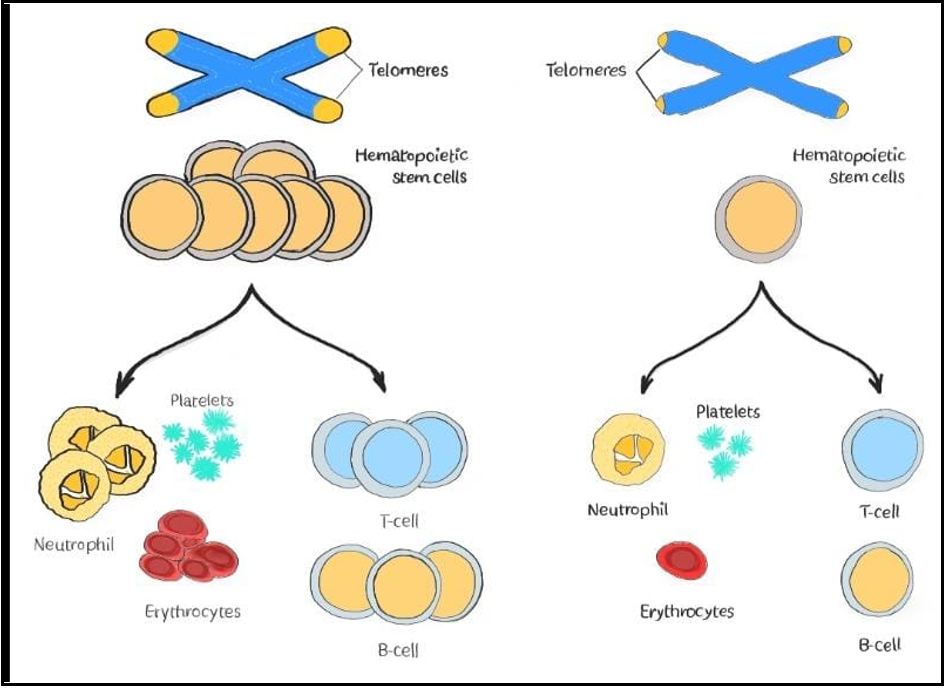
Alcoholic liver cirrhosis (Figure 1) is a chronic liver disease caused by long-term excessive alcohol consumption leading to progressive liver damage and dysfunction. The pathophysiology of alcoholic liver cirrhosis involves multiple complex mechanisms, including oxidative stress, inflammation, altered gut microbiota, and impaired liver regeneration [2]. Alcoholic liver cirrhosis is a progressive disease that results from chronic alcohol abuse and leads to liver damage and scarring. The pathophysiology of alcoholic liver cirrhosis involves multiple mechanisms that can also affect other body organs. Pancytopenia is a common complication of alcoholic liver cirrhosis and can be caused by various mechanisms (Figure 2). According to a study by Goyal et al. (2013), pancytopenia was present in 15.6 % of patients with alcoholic liver cirrhosis and was associated with the worst prognosis. The study found that pancytopenia in alcoholic liver cirrhosis can be caused by decreased production of blood cells in the bone marrow, increased destruction of blood cells in the spleen, and decreased lifespan of blood cells. Another study by Chandra et al. (2008) investigated the mechanisms underlying pancytopenia in alcoholic liver cirrhosis and found that it was primarily due to decreased production of blood cells in the bone marrow and increased destruction of blood cells in the spleen. The effects of pancytopenia on the patient's post-craniotomy and cranioplasty healing process are the primary focus of this paper.
Figure 1: Alcohol induced liver cirrhosis, adapted from smart.servier.com.
Figure 2: Normal Cell differentiation vs Pancytopenia, adapted from smart servier.com
Case Details
A 30-year-old female with a past clinical history of liquor misuse, alcoholic hepatitis, pancytopenia, hyponatremia, liver cirrhosis-prompted hepatic encephalopathy, history of subdural hematoma status post craniotomy and cranioplasty gave liquor inebriation. The patient has been drinking alcohol every other day for 12 years.
Day of admission
Vital signs:
Heart rate (HR) = 80/minute
Respiratory Rate (RR) = 18/minute
Blood pressure (BP) = 94/52 mm of Hg
SPO2: 100 % on room air
Laboratory findings
WBC: 1.8 K/uL
Hemoglobin: 6.1 g/dL
Platelet: 24 thousand/UL
Potassium: 3.2 mEq/L
Alkaline Phosphatase: 170 U/L
AST: 61 U/L
Ammonia level: 105 µ/dL
Management
Alcohol withdrawal:
Monitor CIWA protocol, thiamine folic acid, ativan, elevated ammonia improved with lactulose, counseling for alcohol cessation. Pancytopenia: Improved since admission with blood transfusion subdural hematoma s/p craniotomy & cranioplasty: Monitor healing
Differential Diagnosis
Many causes of chronic liver disease may result in cirrhosis, including chronic viral hepatitis, hemochromatosis, primary biliary cholangitis, primary sclerosing cholangitis, and autoimmune hepatitis [3]. In this case, cirrhosis from binge drinking resulting in pancytopenia is illustrated and should be differentiated from other causes of cirrhosis and pancytopenia.
Discussion
Our patient's case illustrated pancytopenia from hepatic cirrhosis due to loss of thrombopoietin and erythropoietin production, lack of iron storage due to hepatocyte destruction, and splenic sequestration. Pancytopenia corresponds to multilineage cytopenia as thrombocytopenia, leukocytopenia, and erythrocytopenia. Apart from the symptoms of pancytopenia, such as shortness of breath, chest pain, fatigue, effort intolerance, Etc., it significantly affects the wound healing process. Thrombocytopenia causes bleeding and bruising and failed bleeding cessation after the injury, reduced immunity increases the infection attacks from leukopenia, hypoxemia, and hypoxia from erythrocytopenia. So, this patient's post-surgical healing of craniotomy and cranial fasciotomy is challenging.
Clinical observations support that neutrophils are essential for efficient wound repair, as neutropenic individuals often have difficulty healing wounds. Patients with a craniotomy had lower levels of erythrocytes and thrombocytes before surgery, increasing their likelihood of prolonged postoperative hospitalization and requiring more resources. Impairment of leukocyte recruitment is also associated with delayed wound healing. Given the patient's recent craniotomy and cranioplasty, a decrease in neutrophils can also make the patient more susceptible to infections, which can be dangerous [4,5].
Furthermore, decreased thrombocytes can lead to bleeding and bruising, a significant issue in craniotomy wound healing. The patient may experience prolonged bleeding and delayed wound healing, increasing the risk of infection and other complications.
Proper management and treatment of pancytopenia are essential to fasten the patient's recovery and prevent further complications. It is necessary to regularly manage the patient's pancytopenia and monitor the patient's blood cell counts. Blood transfusions, medications that stimulate the production of blood cells, and addressing the underlying cause of pancytopenia, such as chronic alcoholic cirrhosis, are all options for treatment. Considering everything, pancytopenia can influence the injury recuperating process and the general strength of patients with persistent circumstances like ours.
Authors' Contributions: All the authors contributed equally to the case report
Patient consent to publish: The patient's written permission was obtained
Conflict of Interest to Post: Authors declares no conflict of interest to this work
Peer review: External peer review done
Funding: No funding was received
Abbreviations
US: Ultrasound
CIWA: Clinical Institute Withdrawal Assessment
References
- Stages of Cirrhosis - Viral Hepatitis and Liver Disease. (n.d.). Www.hepatitis.va.gov. https://www.hepatitis.va.gov/cirrhosis/ background/stages.asp
- Tilg, H., & Moschen, A. R. (2015). Evolution of inflammation in nonalcoholic fatty liver disease: the multiple parallel hits hypothesis. Hepatology, 62(3), 917-927
- UpToDate.(n.d.).Www.uptodate.com.https://www.uptodate.com/ contents/clinical-manifestations-and-diagnosis-of-alcohol- associated-fatty-liver-disease-and-cirrhosis?search=alcoholic%20liver%20disease&source=search_result&selectedTitle=1~150&usage_type=default&display_rank=1
- Dana, I. M. B. S., Mediana, S., Murti, W. W., & Ariodhanu, W. (2021). Hepatic cirrhosis causes pancytopenia: a case report. International Journal of Advances in Medicine, 8(2), 276. https://doi.org/10.18203/2349-3933.ijam20210275
- Pancytopenia: Symptoms, causes, and treatment. (2017, November 19). Www.medicalnewstoday.com. https://www.medicalnewstoday.com/articles/320075#causes