Tayyab Saeed Akhter1, Sameen Abbas2*, Gul Nisar1, Muhammad Umer1, Hammama-tul-Bushra Khaar1, Javeria Zahid Khan1, Sadia Ahmad1, Abdul Samad2
1Center for Liver and Digestive Diseases, Holy family Hospital Rawalpindi, Pakistan
2Department of Pharmacy, Quaid-I-Azam University, Islamabad
*Corresponding Author: Sameen Abbas, Department of Pharmacy, Quaid-I-Azam University, Islamabad.
Abstract
Ineffective Motility (IM), under the umbrella of the Chicago classification version 3.0 metric, cannot individually define the severity of patient symptoms and clinical outcomes. In light of this, an updated CCv4.0 protocol is proposed with rapid drink challenge (RDC), an effective diagnostic tool that entails better results on high-resolution manometric (HRM) findings and helps redefine cases of patients presenting with IM. We offer a case where a patient with IM, as observed by just manometric findings, was directed for a rapid drink challenge (RDC) test where pan esophageal pressurization and an increase in integrated relaxation pressure (IRP) of 26 mmHg on HRM color contour was observed. Thus, it shows that RDC is an efficient test that can be used to differentiate various groups of esophageal motility disorders, and along with that, it may help medical practitioners diagnose and manage related patients better.
Keywords: Ineffective motility; Achalasia; Esophageal challenge test; High-resolution esophageal manometry; Rapid Drink Challenge
Introduction
High-resolution manometry (HRM) and pressure topography were developed in the twentieth century for the clinical assessment of esophageal motility, which implied a significant advancement in the research opportunities for esophageal motility disorders in clinical practice [1]. New metrics named Chicago Classification were published in 2008 that differed from conventional protocol, i.e., performing manometry with 10 single bolus swallows, administered at 20–30 s intervals, with the patient lying supine [2]. However, some failures to question esophageal function during manometry studies may account for the fact that many incorrect diagnoses, depending on the Chicago Classification, do not indicate the severity of the patient's symptoms or the management changes needed for patients. So, for standardization of findings, a revised version of the Chicago classification system (version 4.0) is proposed, under which categorization of esophageal motility disorders has become easy and simultaneously more insight into the pathophysiology and inter- connection amongst different motility disorders is possible. The protocol, as suggested for the Chicago Classification system v4.0, entails a baseline period of 30 seconds (exclusive of swallowing) in the recumbent position, followed by ten 5-ml swallows and 2 sequences of multiple rapid swallows (MRS), which consist of five 2-ml swallows spaced no more than 2 seconds apart. The participant's position then shifted to a seated position, and five 5-ml swallows were administered, followed by a rapid drink challenge (RDC) test, which involved ingesting 200 ml of water as fast as possible [3].
Multiple swallows, like RDC, are an effective tool for examining the esophagus's inhibitory and excitatory processes. 200 mL of water should be freely consumed as quickly as possible to evaluate the esophagogastric junction (EGJ) [4]. The rapid drink challenge increases peripheral and central deglutitive inhibition, suppressing esophageal body contractions and completely relaxing the lower esophageal sphincter (LES). After contraction, an enhanced peristaltic and LES activity may come after the last swallow. As a result, an abnormal response entails either a peristaltic contraction or an incomplete inhibition of EGJ during swallows and an eccentric contraction following swallows. According to preliminary research, this supplemental test may present a clinically significant obstacle that heightens the sensitivity of HRM studies for identifying esophageal motility disorders, particularly those connected to EGJ dysfunction [5].
Ineffective Motility (IM), despite its much more stringent definition, i.e., >70% inadequate or >50% absent swallows, is the loosest category amongst all that still needs further sub-grouping and deeper insight [6]. Although a separate entity, Achalasia ultimately requires absent peristalsis as one of the criteria to satisfy its diagnosis [7]. In light of this, we present a case where a patient with manometric findings that were consistent with IM underwent a rapid drink challenge test and was transformed topographically into a pattern consistent with Achalasia.
Case presentation
We share a case of a 60-year-old man who presented with dysphagia to solids and liquids for 3 months. He underwent upper GI endoscopy with no evidence of mechanical obstruction and rather vigorous peristalsis with pooling of saliva. HRM showed 60% absent peristalsis and 40 % weak peristalsis. The median IRP for 4 seconds was 7.8 mmHg (Normal <15 mmHg). At the end of the study, a 200 ml rapid drink challenge test was performed that not only changed the pattern of swallows to loss of peristaltic activity and led to pan esophageal pressurizations but raised the IRP to 26 mm of Hg. Patient Eckardt scored 7/12 (Dysphagia 3, Weight Loss 3, Regurgitation 1, Chest pain 0), and a diagnosis of Achalasia was established. The patient was offered different therapeutic options, and the pros and cons were explained. The patient opted for Pneumatic balloon dilatation. Achalasia dilatation was performed using a 30 mm Achalasia balloon with a PSI of 7. On post-procedure follow-up of 1 year, the patient's symptoms have improved with an Eckardt score of 1, and he is doing fine.
Manometric interpretation
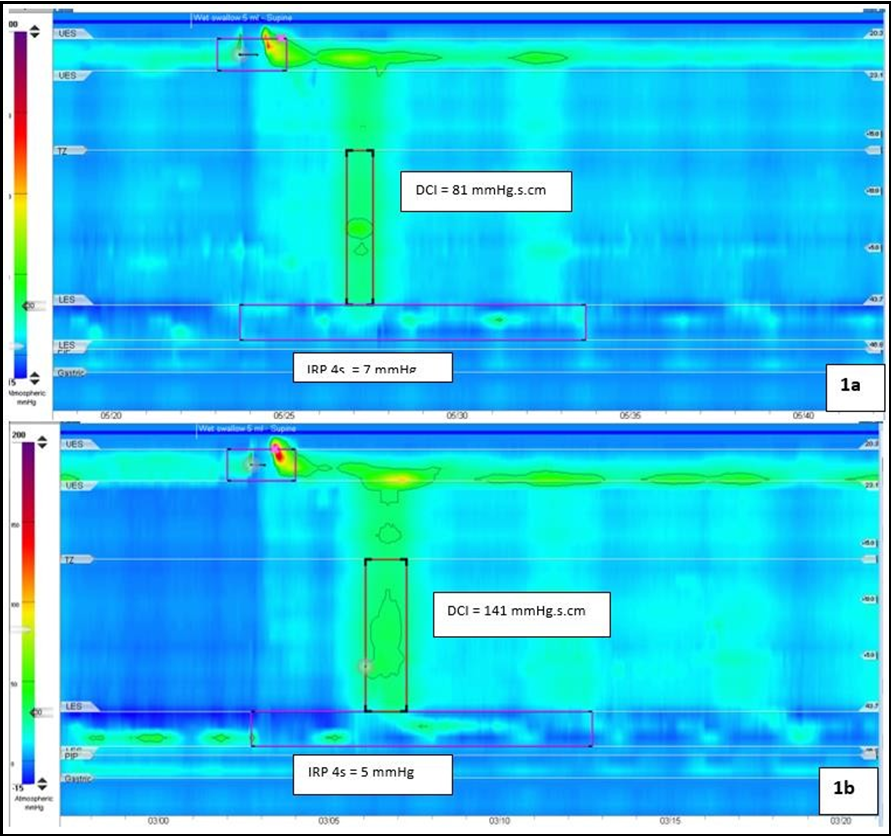
The patient was evaluated on HRM earlier, having consistent IM (Fig 1), where findings suggested wet swallows along with absent peristalsis with DCI <100mmHg.cm.s and weak peristalsis having DCI of 100-450 mmHg.cm.s has been depicted in Figure 1. Integrated relaxation pressure IRP with all swallows was <15 mmHg with a median IRP of 7.8, which made an overall conclusion for patients having 60% absent peristalsis (<100) and 40% weak peristalsis.
Figure 1: An HRM color contour showing wet swallows with absent peristalsis having DCI <100 mmHg.cm.s (a) and weak peristalsis having DCI between 100-450 mmHg.cm.s (b) IRP 4s = 26 mmHg.
Rapid Drink Challenge
The patient was then subjected to a “Rapid drink challenge test” (RDC) with 200ml of water, and recordings were made on HRM contrast (Fig 2) that demonstrated almost loss of peristaltic activity been replaced by pan esophageal pressurization pressure where Integrated relaxation pressure (IRP) was recorded to be 26 mmHg.
Figure 2: An HRM color contour after a rapid drink challenge (RDC) of 200 ml water showing almost loss of peristaltic pattern and being replaced by a pan esophageal pressurization pattern. The Integrated Relaxation pressure (IRP) during the RDC is 26 mmHg.
Discussion
With the advancement of manometric evaluation based on High- resolution technology (HRM), comprehension of the physiology of the esophagus has been made more efficient compared to previous manometric assessment and diagnostic procedures for disorders related to esophageal functions [1]. On the other hand, the Chicago classification system remains standard and is based on HRM that can provide in-depth detail and findings compared to previous criteria [8]. Diagnosis is made according to the Chicago classification, where the protocol is set on ten 5ml swallows in a supine position [2]. But current classification protocol may not give in-depth patterns where motility sustains in most cases. Along with Chicago classification, many other tests may be employed for better comprehension of esophageal patterns and muscular tone, like the Rapid Drink Challenge test (RDC), solid/semisolid swallows, and multiple swallows tests that can help physicians to better assess the condition as compared to using manometric evaluations alone [2], [9].
A powerful peristaltic sequence has been described to follow the rapid drink test in healthy controls, and numerous studies have emphasized the significance of this contraction as a measure of peristaltic reserve in individuals with IM. Fornari et al. reported that approximately fifty percent of patients with IM during single swallows could normalize contractions after RDC, as in our case, using conventional manometry. According to Chicago version 3 research, approximately 50% of healthy, asymptomatic controls with normal single-swallow HRM had a regular peristaltic contraction after multiple swallows, while the other 50% did not have a rebound contraction [10].
Also, RDC is considered to be a better parameter as compared to conventional manometric evaluation because Integrated relaxation pressure (IRP) is a better indicator to show resistance to esophageal emptying due to EGJ and gives better results as compared to IRP been obtained for other parameters that show its sensitivity and specificity in estimating outflow obstruction. At the same time, assessing relationships between different situations predicts a better clinical outcome of the parameter. It can be summarized as mean IRP during RDC depicts predominant clinical features and shows outstanding contrast of esophageal gastro junctional obstruction (EGJO), achalasia, and other disorders of esophageal dysfunction like IM as compared to conventional techniques like timed barium esophagomanometry (TEM) or HRM alone [11].
So, the clinical relevance of this case report is remarkable, the different pressure patterns observed after RDC help finalize doubtful diagnoses, as observed after standard single swallows in HRM, as occurred here with borderline motility disorders, i.e., achalasia and IM. Adding this basic and well-tolerated test to the usual HRM protocol allows for detecting abnormal pressure responses associated with esophageal symptoms but with normal manometry when using the single-swallow protocol. Depending on the precise pressure pattern, RDC will direct more precisely towards particular motor disorders, such as obstructive disorders with sustained pressurization and an increased pressure gradient across the EGJ or non-obstructive disorders with a failure in the inhibitory pathways.
Conclusion
In conclusion, in patients who have clinical signs of altered esophageal motility but normal HRM, it has been noted that pressuretrends in response to a rapid drink challenge test can distinguish between various groups of esophageal motility disorders and identify abnormal motor responses. As a result, this easy and well-tolerated test may help medical practitioners better diagnose and treat those with esophageal motility disorders.
References
- Ayazi S, Crookes PF (2010) High-resolution esophageal manometry: using technical advances for clinical advantages. J Gastrointest Surg. 14(Suppl 1): S24–32.
- Marin I, Serra J (2016) Patterns of esophageal pressure responses to a rapid drink challenge test in patients with esophageal motility disorders. Neurogastroenterol Motil. 28(4): 543–553.
- Sharma P, Yadlapati R (2022) Evaluation of Esophageal Motility and Lessons from Chicago Classification version 4.0. Curr Gastroenterol Rep. 24(1): 10–17.
- Leopold A, Yu D, Bhuta R, Kataria R, Lu X, et al. (2019) Multiple rapid swallows (MRS) complements single-swallow (SS) analysis for high-resolution esophageal manometry (HREM). Dig Dis Sci. 64(8): 2206–2213.
- Ang D, Hollenstein M, Misselwitz B, Knowles K, Wright J, et al. (2017) Rapid drink challenge in high‐resolution manometry: an adjunctive test for detection of esophageal motility disorders. Neurogastroenterol Motil. 29(1): e12902.
- Kurin M, Adil SA, Damjanovska S, Tanner S, Greer K (2023) Clinical Characteristics of Patients With Ineffective Esophageal Motility by Chicago Classification Version 4.0 Compared to Chicago Classification Version 3.0. J. Neurogastroenterol Motil. 29(1): 38–48.
- Yadlapati R, Pandolfino JE, Fox MR, Bredenoord AJ, Kahrilas PJ (2021) What is new in Chicago Classification version 4.0? Neurogastroenterol Motil. 33(1): e14053.
- S Roman S, Gyawali CP, Xiao Y, Pandolfino JE, Kahrilas PJ (2014) The Chicago classification of motility disorders: an update. Gastrointest Endosc Clin. 24(4): 545–561.
- Carlson DA, Roman S (2018) Esophageal provocation tests: are they useful to improve diagnostic yield of high resolution manometry? Neurogastroenterol Motil. 30(4): e13321.
- Fornari F, Bravi I, Penagini R, Tack J, Sifrim D (2009) Multiple rapid swallowing: a complementary test during standard oesophageal manometry. Neurogastroenterol Motil. 21(7): 718- e41.
- Blam ME, Delfyett W, Levine MS, Metz DC, Katzka DA (2002 ) Achalasia: a disease of varied and subtle symptoms that do not correlate with radiographic findings. Am J Gastroenterol. 97(8): 1916–23.