Diana Hodgins*, Jack Newby
Dynamic Metrics Limited, Codi cote Innovation Centre, St. Albans Rd, Codi cote, Herts SG4 8WH, UK
*Corresponding Author: Diana Hodgins, Dynamic Metrics Limited, Codicote Innovation Centre, St. Albans Rd, Codicote, Herts SG4 8WH, UK
Abstract
Considerable evidence now documents that the most effective and cost-effective fall reduction programs involve targeted interventions and exercise programs. Most falls are associated with one or more risk factors, including muscle weakness and gait deficiency.
Clinical gait analysis remains highly observational and is hence subjective and influenced mainly by the observer’s background and experience. For technological advances in gait assessment to be realized in a clinical setting, it is essential that clinical protocols are standardized and that the complex features of human gait can be captured and represented in a format that is meaningful to the patient and the clinician. Exercise prescription also suffers the same subjective influence, in the eye of the beholder, based on the prescriber’s background and experience.
The overall aim of this project was to test both the delivery model and evaluate the impact of the 4-session GaitSmart Rehabilitation program, run over 12 weeks, on patient health outcomes. At an average age of 80, participants were at risk of falls and regular attendees at the NHS GGC Community Falls Prevention Programme Strength & Balance or Bone Health Classes.
The results show that participants improved their gait kinematics, which increased speed. The improvement and the corresponding increase reduce the patient’s risk of poor health outcomes and falls. This also resulted in a reduction in their fear of falling and frailty score and an increase in their quality of life. All of these changes were statistically significant.
Introduction
Falls are a common and often devastating problem among older people, causing a tremendous amount of morbidity, mortality, and use of health care services. In the UK, the government Office for Health Improvement and Disparities (OHID) reported through The Public Health Outcomes Framework (PHOF) that from 2017 to 2018, there were around 220,160 emergency hospital admissions related to falls among patients aged 65 and over, with about 146,665 (66.6%) of these patients aged 80 and above [1]. Most of these falls are associated with one or more risk factors, including muscle weakness and gait deficiency. Research has shown that focusing on these risk factors can significantly reduce falling rates. Considerable evidence now documents that the most effective and cost-effective fall reduction programs involve targeted interventions and exercise programs [2]. Exercise has been shown to affect the physiological systems of the human body, including the brain, endocrine system, immune system, and skeletal muscle [3,4,5,6,7,8]. It has been proven that exercise is an efficient intervention for frail older people to elicit positive health outcomes in mobility and functional ability [8,9,10,11]. Despite numerous studies claiming superiority and popular trends, the most effective intensity (duration and frequency) of an exercise intervention for the population remains to be determined. Adherence across a spectrum of exercise interventions is characteristically high [8].
Frailty is one of the most problematic conditions of population aging. In a systematic review, the average frailty prevalence rate was 9.9% (95% CI 9.6-10.2), and 44.2% for pre-frailty prevalence (95% CI 44.2-44.7). Frailty was statistically more prevalent in women (11 studies, 9.6%, 95% CI 9.2-10) than men (5.2%; 95% CI 4.9-5.5), and frailty increased steadily with age: 65-69 years: 4%; 70-74 years: 7%; 75-79 years: 9% 80-84 years: 16%; >85 years: 26% (12). It is a state of vulnerability that can lead to minor stressor events, triggering disproportionate changes in health status. Appropriate measures of frailty can enable timely intervention and proper goal-driven care (8). Fear of falling (FOF) is an essential threat to autonomy, prevalent among older adults, and associated with adverse health outcomes [13,14]. Exercise intervention programs have been shown to reduce fear of falling and identified as a core metric when evaluating the effectiveness of exercise interventions [15].
Identifying gait variables in older people can be essential to recognize gait deficits and initiate the appropriate treatment [16]. There is an increased risk of multiple falls in older people with poorer gait [17], and stride length may predict future falls in older adults [18].
One analysis revealed that when sex, age, and biomechanical parameters are added to gait, speed prediction of both falls and mortality is significantly improved [19]. Individuals with reduced knee ROM during obstacle-free walking may have more incredible difficulty avoiding obstacles [20].
Clinical gait analysis remains highly observational and is hence subjective and primarily influenced by the observer’s background and experience. Imperative to technological advances in gait assessment is the standardization of clinical protocols and the feasibility of mapping the complex features of human gait while representing them meaningfully to the patient and the clinician [21]. Exercise prescription also suffers the same subjective influence, in the eye of the beholder, based on the prescriber’s background and experience.
Overview of GaitSmart
To address this challenge, NHS Greater Glasgow & Clyde piloted the GaitSmart rehabilitation program, which combines gait analysis and an exercise rehabilitation program. A sensor-based gait assessment system developed by Dynamic Metrics that objectively measures key gait parameters in a short walking test.
GaitSmart tests provide clinicians and patients with critical gait markers such as hip and knee angle, symmetry of movement, and stride duration. How these measurements compare to the healthy reference is indicated in the report using a simple traffic light system. This helps to locate the cause of gait problems and their severity. This objective digital data quantifies subtle changes over time, demonstrating the effectiveness of the intervention program. It can also motivate patients to continue exercising.
The GaitSmart report generates suggested exercises in everyday use throughout the NHS matched to the gait abnormalities identified.
The GaitSmart Programme has improved risk factors such as frailty and fear of falling [22,23]. The gait analysis provides an objective report on the mobility of an individual, which will identify areas of issue in the patient’s mobility and the severity; these quantitative gait markers are independent predictors of falls in older adults, including gait speed [24]. The GaitSmart report uses traffic light coding to identify how far each parameter deviates from normal. It is a proven method to empower and motivate patients in other healthcare applications [25]. The exercise selection is personalized to the patient’s gait to improve the muscle weakness risk factor [22].
Study aims:
The overall aim of this project was to test both the delivery model and evaluate the impact of the GaitSmart Rehabilitation program on patient health outcomes. Does the GaitSmart Rehabilitation Programme reduce the risk of falls in conjunction with fall prevention or bone health classes?
1. Identify whether community exercise classes are suitable for delivering the GaitSmart Rehabilitation Programme for fall risk reduction, monitoring dropout rate, adherence, and patient outcome.
2. Evaluate the impact of using the GaitSmart Rehabilitation Programme on gait and patient outcomes: Gait Speed, GaitSmart Score, Falls Efficacy Scale Questionnaire (FES-I), Edmonton Frailty Score (EFS), and Quality of Life (EQ5D).
Method
Participant Selection
Participants were drawn from regular attendees at the NHS GGC Community Falls Prevention Programme Strength & Balance and Bone Health Classes. Priority was given to volunteers whose circumstances conform to the selection criteria.
Inclusion – participants will have one of the following as a primary condition:
- has fallen.
- at risk of falling
- has a fear of falling.
- gait deficiency
- reduced mobility
You must also be mobile and able to do gentle exercise. Walking aids may be used.
Exclusion – participants with any of the following conditions could not participate:
- the unstable cardiac, respiratory, or neurological condition
- severe cognitive impairment
- skin condition
- infectious disease
- unable to mobilise.
- stroke patient
Before joining the Trial, each participant was required to give their informed consent.
Trial Assessments
The trial assessments occurred during the regular Strength, Balance, and Bone Health Classes. They were managed and carried out by a contracted GaitSmart Support Worker under the direction of an attending NHS physiotherapist.
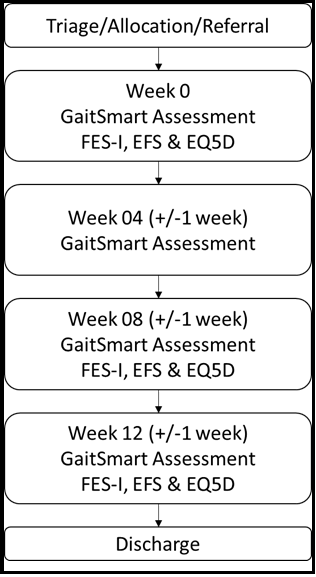
Participants received an assessment at 0 (baseline), 4, 8, and 12 weeks.
Figure 1: GaitSmart Rehabilitation Programme four-session protocol and theoretical care pathway framework.
At the first assessment, by the data security protocol, the participant was assigned a trial ID. This unique identifier served to anonymize the participant for the trial. The following personal details were recorded in the GaitSmart trial database against the trial ID:
- gender
- year of birth
- height
- weight
- employment status
- relevant medical history:
- use of walking aids
- occurrence of falls or trauma
- knee or hip surgery
At each assessment, the GaitSmart Support Worker:
- recorded any changes to medical history, including date and details
- attached the straps and sensors to the participant – this was done over clothing
- asked the participant to stand still for 10 seconds to calibrate the sensors
- asked the participant to walk in a straight line for 10-15 strides, turn around, and walk back to their starting point
- removed the straps and sensors from the participant
- generated the GaitSmart report (analysis of the participant's gait)
- generate suggested exercises
The GaitSmart Support Worker reviewed the report and suggested exercises with the participant and the assigned NHS physiotherapist. The participant was asked to follow the recommended practices at home until the next trial assessment.
At the first, third, and last appointments, the GaitSmart Support Worker worked with the participant to complete three standardized questionnaires, each of which supports the evaluation of the trial outcomes:
- Short Falls Efficacy Scale-International (FES-I) – indicates whether frailty has reduced
- The Edmonton Frailty Scale (EFS) – suggests any reduction in the fear of falling
- EQ-5D – means whether Quality of Life has improved
GaitSmart Support Worker
The GaitSmart Support Worker worked under the direction of the attending NHS physiotherapist(s). The safety of all participants was the responsibility of NHS GGC.
The GaitSmart Support Worker was thoroughly trained in the equipment and trial methodologies.
GaitSmart
GaitSmart is a registered Medical Device where the sensor's accuracy has been determined by the National Physical Laboratory [26], and the system has been compared against the reference standard optical gait lab data in measuring gait kinematics [27,28,29]. GaitSmart comprises seven sensor modules, custom elasticated straps, a tablet, and a carrying case.
GaitSmart test protocol
To deliver the intervention, a 10 m quiet (discrete) straight corridor was used, and patients wore flat or low-heeled shoes with proper support and were instructed to use the same footwear at each appointment, wherever possible. Elasticated straps were applied around the hips, with pockets at the base of the spine and just above the iliac crest, the thigh, just below the greater trochanter, and the belly of the gastrocnemius muscle of the calf (see Figure 2).
Figure 2: Straps attached with sensors mounted.
Exercises
For the GaitSmart intervention programme, six exercises were automatically chosen from the list in Table 1 that best addressed the muscle weakness in the gait deficiency demonstrated by the patients gait assessment. The patient was advised to use support, if required. The patient is given the freedom of choice to decide the frequency, duration and intensity of the exercises. Each patient is guided through their six personalised exercises by the Healthcare Assistant and advised to: 1) ‘Fit the exercises into their daily routine’. 2) ‘Complete as many as you feel comfortable, if any pain or discomfort, stop’.
Table 1: Exercise selection list.
|
No. |
Exercise |
|
1 |
Lunges |
|
2 |
Reverse lunges |
|
3 |
Single leg balance (knee straight) |
|
4 |
Single leg balance (knee bent) |
|
5 |
Knee extensor strengthening in standing |
|
6 |
Standing with weight transfer |
|
8 |
Marching on the spot |
|
9 |
Single leg squat |
|
10 |
Double leg squat |
|
11 |
Hip abduction (1 leg standing) |
|
12 |
Heel (calf) raise (unilateral) |
|
13 |
Straight leg raises forward |
|
14 |
Standing hamstring curls |
|
15 |
Side stepping |
|
16 |
Straight leg raises reverse |
|
17 |
Unilateral pelvis raise |
|
18 |
Hip extension (bent knee) |
|
19 |
Hip flexion (bent knee) |
|
20 |
Toe raises |
|
21 |
Heel to toe walking |
|
22 |
Toe walking |
|
23 |
Heel walking |
|
24 |
Stand on toes |
|
25 |
Quadriceps stretch |
|
26 |
Hamstring stretch |
|
27 |
Calf stretch |
Outcome measures
Gait Speed
Gait speed with established values for Mean Detectable Change (MDC) of 0.05m/s and minimally clinically significant change of 0.1m/s [30,31].
Knee angle
In gait kinematic parameters, knee angle is the combined range of motion through the gait cycle for the left and right knees [28].
A quantifiable increase demonstrates an improvement in hip and knee range of motion.
GaitSmart Score
GaitSmart score, a proprietary value that summarises the limb movement in the sagittal plane, is about a healthy, age-matched control reference (28). A perfect score of 100% is obtained when all parameters are in the normal healthy zone.
Falls Efficacy Scale Questionnaire (FES-I)
The FES-I has close continuity with the best existing measure of fear of falling, excellent psychometric properties, and assesses concerns relating to basic and more demanding activities, both physical and social. It considers the level of worry about slipping when carrying out each activity on a four-point scale from 1=not at all concerned to 4=very concerned [32].
Edmonton Frailty Score (EFS)
The EFS is associated with several geriatric conditions such as independence, drug assumption, mood, mental, functional, and nutritional status, and the EFS appears to be valid, reliable, and feasible for routine use by non-geriatricians [33]. The EFS consists of nine domains and eleven items, each scoring 0 points (frailty absent or normal health), 1 point (minor errors or mild/moderate impairment), or 2 issues (critical errors or severely impaired).
EQ-5D-5L
The EQ-5D-5L is a two-part self-report questionnaire comprising five domain questions (mobility, self-care, usual activities, pain/discomfort, and anxiety/depression) and a visual analog scale of their overall health (VAS). Responses to the domain questions are profiled and mapped [34,35,36] to derive a single index utility value, which reflects quality of life according to the preferences of the general population of a country/region. The Utility index can range from below 0 (a state worse than death) to 1, the value for total health.
Results
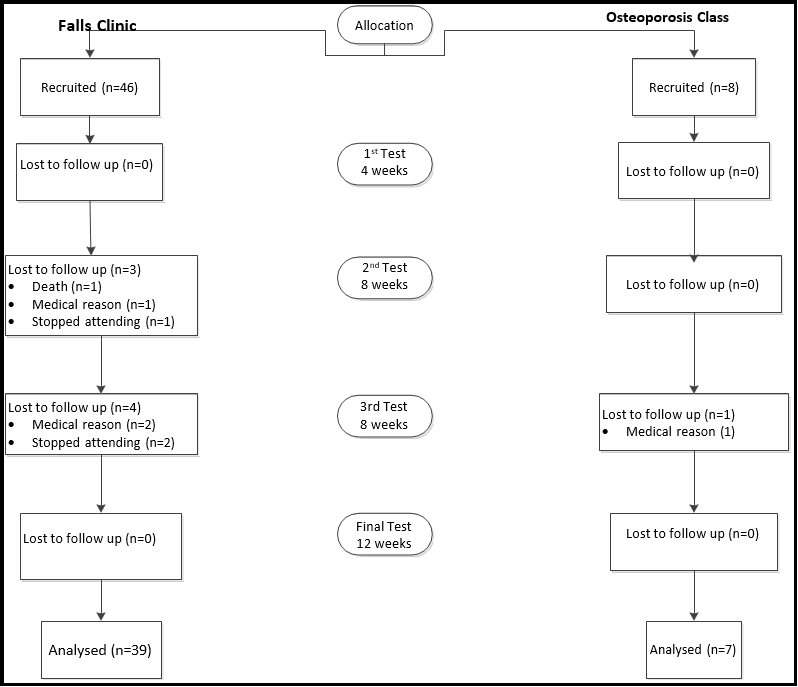
In total 54 patients were recruited; 46 from the Community Falls Prevention Programme and eight from the Osteoporosis Bone Health Class.
Consort Diagram
In total, 54 were recruited and 46 completed the four-session programme, with only 3 withdrawals without a medical reason. Both the falls and osteoporosis patient groups were combined for the analysis.
The patient characteristics of those who completed four tests are summarised in Table 2.
Table 2: Patient characteristics for those who completed the four session study.
|
Number of patients recruited |
54 |
|
Number of patients completed four sessions |
46 |
|
Attrition rate |
13.4% |
|
Adherence rate |
100% |
|
Average Age |
80 |
|
Gender (% female) |
68 |
|
Average BMI |
26.2 |
Table 3. provides a baseline and final values for the objective data and patient questionnaires: FES-I, EFS and EQ5D-3L.
Table 3: Changes in gait and PROMS
|
|
|
Speed (m/s) |
Gait Score (%) |
Knee Angle (°) |
FES-I |
EFS |
EQ5D Index |
EQ5D VAS |
Walking aid |
|
Start |
Ave (SD) |
0.62 (0.19) |
42. 9 (23.9) |
48.1 (9.7) |
11.76 (3.28) |
4.54 (1.77) |
0.80 (.09) |
73.07 (15.85) |
1.5 (0.6) |
|
End |
Ave (SD) |
0.73 (0.21) |
59.1 (25.55) |
54.3 (9.1) |
9.11 (1.77) |
3.2 (1.94) |
0.84 (0.08) |
79.7 (13.44) |
1.5 (0.6) |
|
|
P-Value |
0.0075 |
0.00227 |
0.00205 |
5.74E-06 |
0.0012 |
0.0033 |
0.00024 |
1 |
P value < 0.01 in bold
The increase in gait speed of 0.11 m/s was statistically significant and greater than the minimally clinically considerable change of 0.1m/s [30].
The GaitSmart score relates to how hip and knee movement in the sagittal plane compares to a healthy reference. This reduction in the severity of 16.2% was statistically significant.
The change in knee angle of 6.2° is statistically significant and brings it to around 1SD from the healthy reference value for 70-79-year-olds and comparable for those over 80s [28].
Fear of falling (FES-I) was reduced by 2.65, with 74% reducing their anxiety by the end of the program. This statistically significant reduction brought the average to the lower margin of moderate fear. The frailty score (EFS) was reduced by 1.34, which was statistically significant.
While, on average, the patient group was not considered frail at the outset, this reduction moves them further from being considered invalid.
The EQ5D Index increased by 0.04, and the EQ5D VAS increased by 6.63. Both of these changes were statistically significant.
On average, 50% used a walking stick at the start of the study. Over the trial period, 2 patients reduced from a post to no aid, and two worsened from no assistance to a stick. The net result was no change.
Discussion
Overall, both patient groups engaged in the GaitSmart intervention program in addition to attending their falls clinic or osteoporosis class. The expected high adherence rate and relatively low attrition prove that the GaitSmart Rehabilitation Programme can be placed in the care pathway when attending a class.
The results show that participants improved their gait kinematics, which increased speed. This also resulted in a reduction in their fear of falling and frailty score and an increase in their quality of life. All of these changes were statistically significant.
The improvement in gait kinematics and the corresponding increase in gait speed reduces the patient’s risk of poor health outcomes and falls [38]. This equates to an improvement in EQ5D data and a reduction in the frailty score. The decline in frailty would have reduced adverse outcomes [8]. The decrease in fear of falling is associated with a reduced number of falls and increased activities of daily living [38]. However, because there was no standard care group that only received class exercises, it was impossible to determine how much of the improvement was due to the GaitSmart intervention.
Referring to the patient outcomes, these are comparable to other studies involving GaitSmart interventions [23], where patients only received the GaitSmart intervention program. Gait Speed as the primary outcome measure is a relative increase above the 0.1 m/s substantial change threshold [31] against the 0.16m/s rise shown in [23].
This suggests that, as the GaitSmart Programme is shown to improve patient benefits as a standalone intervention [23], the evidence does not support that combined intervention of the GaitSmart Rehabilitation Programme and Standard of Care would provide augmented outcomes. As the study does not identify how much of the products are influenced by the intervention or standard of care, there is an opportunity to confirm this through further investigation.
Conclusions
Patients who completed the four-session GaitSmart intervention program alongside the exercise classes improved their gait characteristics. They also reduced their fear of falling, their quality of life, and a reduction in their frailty score.
Limitations of the study
There was no control group, where patients were monitored but not provided with their GaitSmart report and exercises.
These patients also attended the Community Falls Prevention Programme or the Osteoporosis Balance and Bone Health Classes. It is therefore not possible to ascertain what benefits they would have obtained from the classes alone.
Acknowledgements
The trial was conducted within the NHS of Greater Glasgow and Clyde Community Falls Prevention or Bone Health Programme.
References
- Office for Health Improvement and Disparities (2022) Falls: applying All Our Health.
- Rubenstein LZ (2006) Falls in older people: epidemiology, risk factors and strategies for prevention. Age and ageing. 35(Suppl 2): ii37–ii41.
- Singh MA, Ding W, Manfredi TJ, Solares GS, O'Neill EF, et al. (1999) Insulin-like growth factor I in skeletal muscle after weight- lifting exercise in frail elders. The American journal of physiology. 277(1): E135–43.
- van Praag H (2009) Exercise and the brain: something to chew on. Trends in neurosciences. 32(5): 283–290.
- Barber SE, Clegg AP, Young JB (2012) Is there a role for physical activity in preventing cognitive decline in people with mild cognitive impairment? Age and ageing. 41(1): 5–8.
- Gleeson M, McFarlin B, Flynn M (2006) Exercise and Toll-like receptors. Exercise immunology review. 12: 34–53.
- Handschin C, Spiegelman BM (2008) The role of exercise and PGC1alpha in inflammation and chronic disease. Nature. 454(7203): 463–9.
- Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K (2013) Frailty in elderly people. The Lancet. 381(9868): 752-62.
- de Vries NM, van Ravensberg CD, Hobbelen JS, Olde Rikkert MG, Staal JB, et al. (2012) Effects of physical exercise therapy on mobility, physical functioning, physical activity and quality of life in community-dwelling older adults with impaired mobility, physical disability and/or multi-morbidity: a meta-analysis. Ageing research reviews. 11(1): 136–49.
- Theou O, Stathokostas L, Roland KP, Jakobi JM, Patterson C, et al. (2011) The effectiveness of exercise interventions for the management of frailty: a systematic review. Journal of aging research. 2011: 569194.
- Clegg AP, Barber SE, Young JB, Forster A, Iliffe SJ (2012) Do home-based exercise interventions improve outcomes for frail older people? Findings from a systematic review. Reviews in clinical gerontology. 22(1): 68–78.
- Collard RM, Boter H, Schoevers RA, Oude Voshaar RC (2012) Prevalence of frailty in community-dwelling older persons: a systematic review. Journal of the American Geriatrics Society. 60(8): 1487–92.
- Denkinger MD, Lukas A, Nikolaus T, Hauer K (2015) Factors associated with fear of falling and associated activity restriction in community-dwelling older adults: a systematic review. Am J Geriatr Psychiatry. 23(1): 72-86.
- MacKay S, Ebert P, Harbidge C, Hogan DB (2021) Fear of Falling in Older Adults: A Scoping Review of Recent Literature. Can Geriatr J. 24(4): 379–394.
- Kendrick D, Kumar A, Carpenter H, Zijlstra GA, Skelton DA, et al. (2014) Exercise for reducing fear of falling in older people living in the community. The Cochrane database of systematic reviews. 2014(11): CD009848.
- Freire Junior RC, Porto JM, Rodrigues NC, Brunelli RDM, Braga LFP, et al. (2016) Spatial and temporal gait characteristics in pre- frail community-dwelling older adults. Geriatrics & gerontology international. 16(10): 1102–1108.
- Callisaya ML, Blizzard L, Schmidt MD, Martin KL, McGinley JL, et al. (2011) Gait, gait variability and the risk of multiple incident falls in older people: a population-based study. Age Ageing. 40(4): 481-7.
- Marques NR, Spinoso DH, Cardoso BC, Moreno VC, Kuroda MH, et al. (2018) Is it possible to predict falls in older adults using gait kinematics? Clinical biomechanics (Bristol, Avon). 59: 15– 18.
- Porta S, Martínez A, Millor N, Gómez M, Izquierdo M (2020) Relevance of sex, age and gait kinematics when predicting fall- risk and mortality in older adults. Journal of biomechanics. 105: 109723.
- Benson LC, Cobb SC, Hyngstrom AS, Keenan KG, Luo J, et al. (2018) Identifying trippers and non-trippers based on knee kinematics during obstacle-free walking. Hum Mov Sci. 62: 58– 66.
- Hulleck AA, Menoth Mohan D, Abdallah N, El Rich M, Khalaf K (2022) Present and future of gait assessment in clinical practice: Towards the application of novel trends and technologies. Frontiers in medical technology. 4: 901331.
- Perell KL, Nelson A, Goldman RL, Luther SL, Prieto-Lewis N, et al. (2001) Fall risk assessment measures: an analytic review, Journals of Gerontology. Series A, Biological Sciences and Medical Sciences. 56(12): M761-6.
- Rodgers G, Mottley A, Hodgins D (2020) Novel Digital Gait Kinematic Solution to Improve Frailty. British Journal of Healthcare and Medical Research. 7(5): 01–10.
- Verghese J, Holtzer R, Lipton RB, Wang C (2009) Quantitative gait markers and incident fall risk in older adults. J Gerontol A Biol Sci Med Sci. 64(8): 896-901.
- Chmiel C, Senn O, Rosemann T, Del Prete V, Steurer-Stey C (2014) CoCo trial: Color-coded blood pressure Control, a randomized controlled study. Patient Prefer Adherence. 8: 1383- 92.
- Heaps J (2019) Inertial Measurement Unit Characterisation for Gait Analysis. 3DMC 2019 Here East, London.
- McCarthy I, Hodgins D, Mor A, Elbaz A, Segal G (2013) Analysis of knee flexion characteristics and how they alter with the onset of knee osteoarthritis: a case control study. BMC Musculoskelet Disord. 14: 169.
- Monda M, Goldberg A, Smitham P, Thornton M, McCarthy I (2015) Use of Inertial Measurement Units to Assess Age-Related Changes in Gait Kinematics in an Active Population. Journal of Aging and Physical Activity. 23(1): 18-23.
- Zügner R, Tranberg R, Timperley J, Hodgins D, Mohaddes M, et al. (2019) Validation of Inertial Measurement Units with Optical tracking system in patients operated with Total Hip Arthroplasty. BMC Musculoskeletal Disorders. 20(1): 52.
- Abellan van Kan G, Rolland Y, Andrieu S, Bauer J, Beauchet O, et al. (2009) Gait speed at usual pace as a predictor of adverse outcomes in community-dwelling older people an international academy on nutrition and aging (iana) Task force. J Nutr Health Aging. 13(10): 881-9.
- Perera S, Mody SH, Woodman RC, Studenski SA (2006) Meaningful change and responsiveness in common physical performance measures in older adults. Journal of the American Geriatrics Society. 54(5): 743–9.
- Yardley L, Beyer N, Hauer K, Kempen G, Piot-Ziegler C, et al. (2005) Development and initial validation of the Falls Efficacy Scale-International (FES-I). Age and ageing. 34(6): 614–9.
- Rolfson DB, Majumdar SR, Tsuyuki RT, Tahir A, Rockwood K (2006) Validity and reliability of the Edmonton Frail Scale. Age and ageing. 35(5): 526–9.
- Pynsent PB, Adams DJ, Disney SP (2005) The Oxford hip and knee outcome questionnaires for arthroplasty. J Bone Joint Surg Br. 87(2): 241-8.
- Hernández Alava M, Pudney S, Wailoo A (2020) Estimating the relationship between EQ-5D-5L and EQ-5D-3L: results from an English Population Study. Policy Research Unit in Economic Evaluation of Health and Care Interventions. Universities of Sheffield and York.
- NICE health technology evaluations: the manual Process and methods (PMG36) Published: 31 January 2022.
- Kerrigan DC, Lee LW, Collins JJ, Riley PO, Lipsitz LA (2001) Reduced hip extension during walking: healthy elderly and fallers versus young adults. Archives of physical medicine and rehabilitation. 82(1): 26-30.
- Li F, Fisher KJ, Harmer P, McAuley E, Wilson NL (2003) Fear of falling in elderly persons: association with falls, functional ability, and quality of life. J Gerontol B Psychol Sci Soc Sci. 58(5): P283-90.
- McNamara I, Whitehouse CE, Ward N, Whalley R, Hodgins D (2023) Pilot randomized trial using sensor data to personalise rehabilitation following joint replacement and compared to Standard of Care, Pilot Randomized Trial. British Journal of Healthcare and Medical Research. 10(5): 54-71.