Homagnissin Benoît Kouwakanou1α, Samah Ali Said1, Nazirathe Cheick1, Osée Armel Yangba-Kalebanga1, Adil Ait Errami1, Sofia Oubaha2, Zouhour Samlani1, Khadija Krati1
1Department of Hepato-gastroenterology, Mohammed VI University Hospital of Marrakech, Morocco.
2Department of Physiology, Faculty of Medicine, Cadi Ayyad University, Marrakech, Morocco.
αCorresponding Author: Homagnissin Benoît Kouwakanou, Department of Hepato-gastroenterology, Mohammed VI University Hospital of Marrakech, Morocco.
Abstract
The colonic hemangiomantosis is a vascular malformation that is a vascular tumor, existing since the embryonic period, and that develops with the size of the body. They have a noisy expression by rectorrhagia of variable abundance most often but also can be asymptomatic and realize a picture of occult bleeding. We report the case of a 55-year-old female patient whose diagnosis of hemangiomantosis was made incidentally following an iron deficiency anemia workup with a Fecale Immuno-chemical Test (FIT) positive. As she did not present any bleeding complications, the therapeutic attitude consisted of martial supplementation followed by clinical and biological monitoring.
Keywords: iron deficiency anemia - positive FIT test - colonic hemangiomatosis - case report
Introduction
Colon hemangiomas are rare, non-malignant lesions arising from submucosal vascular plexuses due to embryonic sequestration of mesodermal tissue [1,2,3]. Hemangiomas, histologically distinct from telangiectasias and angiodysplasias, can be classified as capillary, cavernous, or mixed. Approximately 80 % of hemangiomas of the colon are massive and can be distinguished from the capillary type, which is usually solitary and cause no symptoms. Cavernous hemangiomas comprise large, thin-walled vascular channels and lack a capsule, facilitating their clinical expression as hectography.
The most frequent mode of revelation is rectal bleeding of variable abundance ranging from a small amount to a state of shock [3,4] or anemia in 43 % of cases [3,5].
We report the case of a colonic and hepatic hemangioma revealed by an iron deficiency anemia workup.
Patient and observation
Patient information: This is a patient M. Z, 55 years old, without any particular pathological history, mother of 3 children, housewife with the notion of passive smoking, admitted for etiological assessment of iron deficiency anemia without external bleeding with a Fecale Immuno-Chemical Test (FIT test) positive and evolving in a context of conservation of the general state.
Clinical outcome: The clinical examination showed a patient in good general condition, hemodynamically, and respiratorily stable. The clinical study and pelvic touch are without abnormality.
Diagnostic approach: Biologically, the hemoglobin level was 9.2 g/dl, microcytic hypochromic anemia, ferritin at 13, hematocrit at 26 %, platelets count at 210,000/mm3, vitamin B12 and folate normal, C-reactive protein at 9, liver and kidney function tests were strictly normal
As part of the etiological assessment of this iron deficiency anemia, the patient underwent a:
- The oesogastro duodenal fibroscopy is normal with preserved duodenal folds,
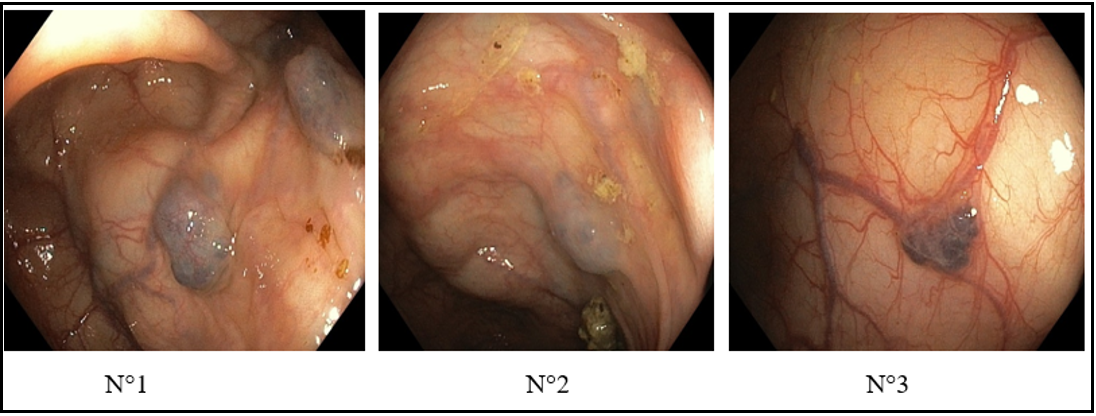
- And a colonoscopy reveals red-blue lesions, giving the appearance of multiple polypoid nodules of variable size, which may be related to a colonic hemangioma and extending from the right colon to the left colonic angle (see figure)
Figure: Colonoscopy image showing colonic hemangioma lesions
N°1: Hemangioma of the left colonic angle
N°2: Hemangioma of the right colon
N°3: Hemangioma of the transverse
- A complimentary endoscopic video capsule to look for localization of angiomatosis lesions in the bowel or other causes of iron deficiency anemia was normal,
- An abdominopelvic CT scan revealed some hemangioma-like liver lesions without any sign of complication and a diffuse nodular parietal thickening in places with calcifications "phlebolith-like" of the colonic frame.
The diagnosis of a colonic hemangioma associated with hepatic hemangioma was retained. This colonic hemangioma would be responsible for probable occult bleeding.
Therapeutic approach: Martial therapy was instituted with clinical-biological monitoring and transit regulation.
A total colectomy was indicated in case of a lower digestive hemorrhage by rupture of these lesions colonic hemangioma (patient in the clear).
Discussion
First described in 1839 [6], hemangiomas constitute 7 % of all benign vascular tumors, are characterized by an increased number of normal or abnormal blood-filled vessels and are usually localized. When they involve many organs in the body, the situation is called angiomatosis or hemangiomatosis [7,8]. In reality, the term hemangioma is used because of the clinical familiarity with the term, but in the true sense, it is a cavernous malformation. The recent classification (revised in 2018) by the International Society for the Study of Vascular Anomalies classifies hemangiomas/cavernous malformations as venous malformations that should be distinguished from hemangiomas [9,10]. Indeed, a hemangioma has a high endothelial cell turnover and is usually present 6 to 8 weeks after birth [11]. They also have a proliferative phase for a few years, usually with spontaneous involution, whereas venous malformations tend to grow proportionately to body size [11].
These malformations can occur at any level of the gastrointestinal tract. The intestinal locations are by far the most frequent [5] and can occur at any age, which would explain certain forms observed in children [5,12]. They can sometimes be associated with specific lesions in certain locations or organs and determine a syndrome (skin, bone, brain, spinal cord, etc.) [5,9] cf. Table 1.
Table 1 : Syndromes that Are Associated with Hemangiomas and Vascular Malformations [5].
|
Syndrome |
Inheritance |
Characteristics |
|
Blue rubber nevus syndrome |
Most sporadic |
Cavernous hemagiomas of the skin, Gastro intestinal tract, and other viscera. Lesions are blue, tender and blanche |
|
Klippel-Trenaunay-Weber syndrome |
Sporadic |
Triad of cutaneous hemangiomas, bone and soft tissue, hypertrophiy of lower extremities, and congenital varicosities |
|
Osler-Rendu-Weber syndrome |
Autosomal dominant |
Mucocutaneous telangiectaias, especially oral and nasalhemangiomatous lesions in stomach, small intestine and rectum |
The frequent mode of revelation is represented by rectal bleeding of variable abundance, which can lead to a misdiagnosis at the beginning [13].
A rigorous interrogation allows us to search for the age of this bleeding and especially the painless character and the recurrence of this rectal bleeding must attract our attention with endoscopic exploration which allows us to make a positive diagnosis. Cases of intestinal obstruction have also been reported regarding polyploid lesions [5,14]. Sometimes it is during the exploration of chronic iron deficiency anemia [5] that the diagnosis is made, as in the case of our patient, but she has the particularity of having a positive FIT test, which indicates occult digestive bleeding. In rare situations, exploring non-gastrointestinal malformations such as hemothorax or hemopericardium leads to diagnosing gastrointestinal hemangioma [5].
The positive diagnosis is made by exploration by lower digestive endoscopy (recto sigmoidoscopy, complete colonoscopy), which allows the topographic diagnosis and extension of the lesions. The endoscopic video capsule represents the gold standard for diagnosing colonic and intestinal hemangiomatosis [4,14]. In our patient's case, the endoscopic video capsule was performed to search for intestinal hemangiomas and the intestinal etiology of iron deficiency anemia. The histology of the resection specimen also allows the diagnosis of certainty of hemangiomatosis [1].
On the imaging level, in typical forms, the pelvic, abdominal CT scan shows a marked thickening of the recto-colonic wall and several abdominal phleboliths [3,8,9]. Phleboliths are pathognomonic signs of hemangiomatosis, but their absence does not rule out the diagnosis [8]. Other explorations, such as MRI, and mesenteric angiography, are sometimes necessary for the diagnosis [8,9].
The management of colonic hemangiomatosis consists, apart from a restoration of the hemodynamic state by blood transfusion or iron infusion, depending on the condition of the patient, then conservative treatment and radical or curative treatment.
Conservative treatments such as sclerotherapy, cryotherapy, embolization, thermoablation, and ligation of lesions may provide only brief control of symptoms [4,9,15,16]. Recent use of medical therapies such as celecoxib, thalidomide, propranolol, and bevacizumab have been used due to their inhibition of vascular endothelial growth factor (VFGF) and fibroblast growth factor (FGF) pathways as well as vasoconstriction, which are shown to be promotive [9].
The best treatment is radical treatment by surgery with excellent results, according to the literature [4,9]. The type of resection is chosen according to the location and degree of disease, relationships with the anal sphincter [4,9,15].
Therapeutic management depends on several factors, including patient preference, the defect's morphology, and the symptoms' severity [9]. As our patient was not bleeding (no external bleeding), the therapeutic attitude was to correct the iron deficiency by per os supplementation, transit regulation, and clinical-biological monitoring was instituted. This attitude seems similar to that proposed by Ganesananthan and al, Abeysekera and al [9,17].
Conclusion
rare etiologies of iron deficiency anemia may be colonic hemangiomatosis. Its frequent mode of revelation is rectal bleeding. Its diagnosis becomes easy with careful questioning and based on lower digestive endoscopy and imaging (abdominal and pelvic CT +/- pelvic MRI). Therapeutic management depends on clinical symptomatology, but the radical and curative treatment remains surgical.
Conflicts of Interest: All authors declare no conflict of interest
Author Contribution: All authors contributed to this work and read and approved the final version of the manuscript.
References
- Wang YA, Ahmad AN (2007) Diffuse Cavernous Hemangioma of the Colon and Rectum. Clin Gastroenterol Hepatol. 5(8): A25.
- Ruiz-Moreno F (1962) Hémangiomatose du côlon. Dis Colon Rectum 5: 453-456.
- Hsu MR, Horton MK, Fishman KE (2002) Diffuse Cavernous Hemangiomatosis of the Colon: Findings on Three-Dimensional CT Colonography. Journal américain de Roentgenology. 179(4): 1042-1044.
- O'farril R, Herrejón JM, Coyoli o, Martinez JM, Toledo CR, et al. (2012) Hemangioma cavernoso de rectosigmoides, enfermedad poco común y mal estudiada. cir gen. 34(1): 65-71.
- Yoo S (2011) GI Associated Hemangiomas and Vascular Malformations, Clinics in Colon and Rectal Surgery. 24(3): 193- 200.
- Phillips B. Surgical cases. London Med Gaz 1839 23: 514–517
- Schoen FJ, Cotran RS (2003) Robbins Basic Pathology. 7th ed. Philadelphia : Saunders.
- Marinis A, Kairi E, Theodosopoulos T, Kondi-Pafiti A, Smyrniotis V (2006) Right colon and liver hemangiomatosis: A case report and a review of the literature. World J Gastroenterol. 12(39): 6405-6407.
- Ganesananthan S, Barlow J, Durai D, Hawthorne AB (2019) Multiple venous malformations in the left colon and rectum: a long-standing case managed conservatively and an update of current literature. BMJ Case Rep. 12(3): e227700.
- Wassef M, Blei F, Adams D, Alomari A, Baselga E, et al. (2015) Vascular anomalies classification : recommendations from the international society for the study of vascular anomalies. Pediatrics. 136(1): e203–e214.
- Mulliken JB, Glowacki J (1982) Hemangiomas and vascular malformations in infants and children: a classification based on endothelial characteristics. Plast Reconstr Surg. 69: 412–22.
- El Bakkaly A, Ettayebi F, Oubeja H, Erraji M, Zerhouni H (2017) Syndrome de Bean chez l’enfant : à propos de deux cas. Pan African Medical Journal. 28: 102.
- Oner Z, Altaca G (1993) Diffuse cavernous rectal hemangioma— clinical appearance, diagnostic modalities and sphincter saving approach to therapy: report of 2 and a collective review of 79 cases. Acta Chir Belg. 93(4): 173–176.
- Ruiz-Cáez K, Cure-Michailith J, Canedo-Matute J, Jiménez- Canedo J (2021) Cavernous hemangioma of the colon in a young patient. Rev Colomb Gastroenterol. 36(1): 93-97.
- Stojčev Z, Maliszewski D, Pawłowska-Stojčev I, Kasprzyk T, Jaśkiewicz J (2013) Diffuse cavernous hemangioma of the rectum (DCHR)--diagnosis and treatment--case report and review of available literature. Pol Przegl Chir. 85(4): 216-8.
- El Mortaji H, Boutakioute B, Ouali Idrissi M, Cherif Idrissi El Ganouni N (2020) Diffuse Cavernous Hemangioma: Rectal Cancer Mimic, Sch J Med Case Rep. 8(10): 904-907.
- Abeysekera KWM, Pearl DS, Burn P, Lowe A (2019) Incidental finding of diffuse cavernous rectal haemangiomatosis during bowel cancer screening. BMC Gastroenterology. 19(1): 198.