Taha Sheikh1, *, Luke Tsai1, Shamis Hasan2, Praful Tewari3, Ragheb Assaly3
1Department of Internal Medicine, University of Toledo College of Medicine, Toledo, Ohio, USA
2 Department of Radiology, University of Toledo College of Medicine, Toledo, Ohio, USA
3 Department of Pulmonology, University of Toledo College of Medicine, Toledo, Ohio, USA
*Corresponding Author: Sheikh T, Department of Internal Medicine University of Toledo College of Medicine, Toledo, Ohio, USA
Abstract
Diagnosis of COVID-19 is an increasingly challenging task during a pandemic where symptoms are beguiling due to a wide array of symptomatology. Radiologic diagnosis plays a vital role not only in diagnosis but in early assessment and triage of suspected patients with COVID- 19 pneumonia. Typically, bilateral ground-glass opacities are considered high-risk and pathognomonic findings for diagnosis. However, COVID- 19 is notorious for varying radiologic presentation as well. We describe a case of cannon-ball appearance of COVID-19 pneumonia which has not been described previously in the literature and is a novel finding.
Keywords: COVID-19, COVID-19 pneumonia, cannon-ball appearance, malignancy
Introduction
Since late December of 2019, the pandemic is known as coronavirus disease 2019 (COVID-19) has been overwhelming healthcare systems globally as it has rapidly spread throughout over 200 different countries. The World Health Organization (WHO) has declared COVID-19 as a Public Health Emergency of International Concern (PHEIC) [1] in January of 2020, and now reports that there are over 40 million confirmed cases with over 1 million deaths worldwide as of October 18, 2020 [2]. COVID-19 patients present with nonspecific symptoms of fever, cough, and shortness of breath, which makes early detection and containment difficult. Even if COVID-19 is suspected early on, the current reference standard for diagnosis is a real-time reverse transcriptase-polymerase chain reaction (RT-PCR), which has shown to yield significant false- negative results [3]. One study reports a high false-negative rate ranging from 68-100 % on the first 4 days of infection prior to symptom onset, dropping only to 21 % one week after infection [4]. Consequently, an alternative modality such as CT imaging for detection and diagnosis may prove to be very valuable for treatment purposes and more importantly, limiting and controlling the spread of COVID-19. Chest CT imaging has the potential to both detect infection and determine its severity according to a series of studies [5]. This alternative method of detection is especially useful in the case of an ambiguous or false-negative RT-PCR result and help validate true-positive results, demonstrated by a study that found 5 of 167 patients with positive chest CT and negative RT-PCR results test positive for COVID-19 days later [6]. According to meta-analyses, COVID-19 on chest CT commonly presents with ground glass opacities in 86% of cases, consolidation in 47 % of cases, and air bronchogram sign in 46 % of cases [7]. By identifying these common patterns and being cognizant of new and potentially coronavirus- specific signs, we hope to add another crucial layer of testing to the diagnostic process of COVID-19.
However, despite the wide array of findings on CT scan, cannon-ball appearance has not been reported per our review of the literature. Cannon-ball appearance in radiology describes the presentation of multiple rounds, nodular opacities with well-defined borders [8]. The most common cause of cannonball appearance is metastatic malignancy; however, other infectious diseases such as pulmonary tuberculosis, histoplasmosis, cryptococcosis, and nocardiosis can also present with granulomas that match this finding [9]. We present a case of a COVID-19 positive patient who misleadingly presented with cannonball appearance on CT scan, causing a management dilemma.
Case
A 35-year-old man with a past medical history of type 1 diabetes mellitus, Factor V Leiden deficiency, and deep vein thrombosis (DVT) (for which he was on anticoagulants with warfarin) presented via Emergency Medical Services (EMS) with altered mental status and respiratory distress. He does not smoke nor drink alcohol and denied fever, chills, cough, sore throat, recent viral illness, recent travel, or sick contacts. He was treated two months prior for sepsis secondary to osteomyelitis of the foot, which he recovered well from on the follow-up visit. On presentation to the emergency department, the patient was noted to be obese, afebrile, tachycardic, hypotensive with a blood pressure of 80/50 mmHg, and tachypneic with 89 % oxygen saturation on room air. He was placed on oxygen by high- flow nasal cannula. A chest exam revealed rhonchi and decreased breath sounds bilaterally. Arterial blood gas test (ABG) showed worsening acidosis with PaO2 at 70 mmHg and PaCO2 at 50 mmHg. He developed grunting respirations and was intubated for airway protection and respiratory distress. Labs showed lymphocytes at 7.5x109/L with lymphopenia of 8.5 %, procalcitonin at 1.72 ng/mL, ferritin at 453 ng/mL, D-dimer at 195 ng/mL, CRP at 10.3 mg/dL, LDH at 403 U/L, lactate at 2.1 mmol/L, and creatinine at 1.45 mg/dL. Troponin and BNP was negative while an echocardiogram (EKG) showed sinus tachycardia. The viral respiratory pathogen panel was negative, and urinalysis was unremarkable. The chest X-ray showed a cannon-ball appearance in all lung fields bilaterally (Figure 1), which was a new finding compared to the normal X-ray from prior admission.
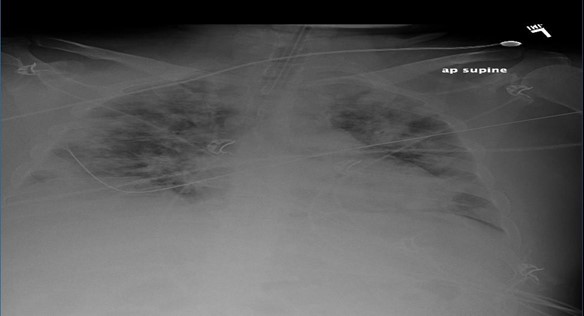
Figure 1: AP Supine chest radiograph showing a mechanically ventilated patient with multifocal bilateral nodular consolidation resembling cannon-ball appearance.
A chest computerized tomography (CT) scan revealed a lack of pleural abnormalities, but prominent rounded densities were displayed throughout all lobes. Most of these were of soft tissue density but some small ground-glass areas were displayed in at least the right middle lobe and both upper lobes (Figure 2 & Figure 3). These cannon-ball opacities were virtually all new since the recent previous CT. Subsequently, the patient tested positive on the RT-PCR for COVID-19. He was then put in contact and airborne isolation in the ICU for further management. He was started on pressor support for his hypotension. The ventilator was set to low tidal volume and high positive end-expiratory pressure (PEEP). He was started on broad-spectrum antibiotics including doxycycline and ceftriaxone. However, he continued to spike fevers and had leukocytosis by the third day. Blood and sputum cultures continued to be negative. The patient was started on redelivering on day 3.
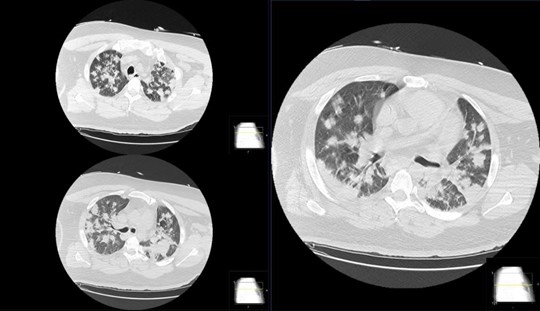
Figure 2: Non-contrasted computed tomography axial images of the chest showing multifocal bilateral nodular consolidations with panlobular affectation and only minimal interspersed ground glass opacities.
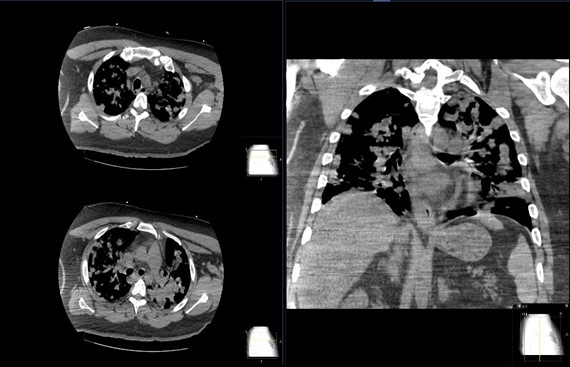
Figure 3: Non-contrasted computed tomography soft tissue window axial and coronal images of the chest showing multifocal bilateral nodularity and consolidation with panlobular affection.
On day 7, he suffered from a seizure episode. Neurology was consulted and brain magnetic resonance imaging (MRI) and video electroencephalogram (EEG) were negative, and the patient was started on levetiracetam. By day 10, his fever, leukocytosis, and procalcitonin started to worsen. Chest X-ray showed basilar airspace density and left pleural effusion. Combined with the persistent fever and leukocytosis, the patient was presumed to have incurred aspiration pneumonia. His repeat sputum cultures from endotracheal (ET) tube grew gram-positive cocci which grew normal flora later. Tuberculosis, fungal cultures, and autoimmune panel were also negative. He was started on ceftriaxone and metronidazole. His fever subsided slowly, and his leukocytosis eventually improved. On day 19, the patient self-extubated. He had a strong cough and copious expectations but was awake, had stable vital signs, was able to follow commands, and did not appear distressed. He was started on oxygen by nasal cannula and recovered well thereafter. He was transferred out of the ICU on day 22 and was out of contact isolation on day 24. On day 30, the patient was discharged on room air. A repeated chest CT showed clearing of the majority of the cannon-ball opacities with minimal remnant nodules (Figure 4). The pulmonary team was recommended to follow up outpatient and repeat chest CT in a few weeks to confirm for resolution. A repeated COVID-19 RT-PCR test was still positive, but the patient was asymptomatic. The infectious disease team cleared him from contact and airborne isolation. He was to follow-up with pulmonology and neurology as an outpatient to repeat chest CT and continue levetiracetam for seizure on discharge. By the 3-month follow-up, the patient had made a complete recovery.
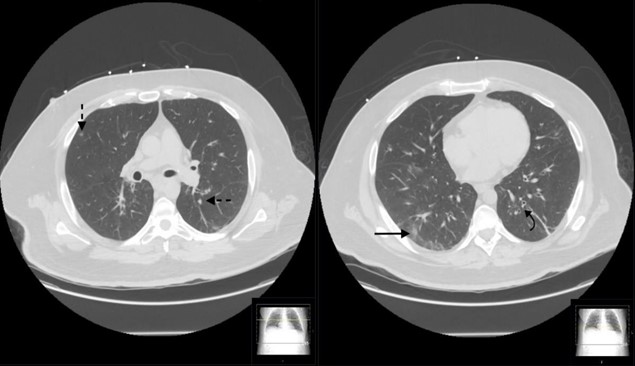
Figure 4: Non-contrasted computed tomography axial images of the chest showing resolving nodularity with some residual ground glass opacity (solid black arrow), pulmonary nodules (broken black arrow) and bronchiectasis (curved black arrow).
Discussion
If CT imaging is to become an essential tool in the diagnostic process of COVID-19, then it is necessary to first understand its different appearances on chest CT. According to one meta-analysis [5], COVID-19 manifests most commonly with bilateral and multilobar lesions, with single lung and lobe lesions presenting less commonly. The most common type of lesion density found was ground-glass opacities, seen in this patient case, followed by air bronchogram signs, crazy-paving pattern, and consolidation. This study also categorized the lesions by shape, where patchy was the most common, followed by spider web sign, cord-like, and nodular, seen in this patient. Other radiological signs that accompanied these lesions were pleural thickening, followed by more rare signs of lymphadenopathy and pleural effusion [5].
Another a meta-analysis on COVID-19, CT manifestations found that nearly 70 % of patients had lesions located in the right lower lobe and that 65 % had 3 or more lobes involved [7]. The infective preference for the right lower lobe is a potential pattern as observed by the study, which becomes important in differentiating it from concurrent aspiration pneumonia. Additionally, the number of affected lobes is potentially significant because it may correlate with the severity and progression of the disease [3]. Similar to the first meta-analysis, this analysis also found that the most common lesion was ground-glass opacities without consolidation, as it affected 86 % of patients [7]. The potential explanation for this common finding is that these patients are either in the early phase of viral infection or that the immune system has successfully limited the spread of disease and absorbed parts of the consolidation area [10]. The ground glass opacities saw in the right lobes of this the patient indicates that his radiological presentation is quite common among COVID-19 patients, aside from his cannon-ball opacities.
In immunocompromised states, the disease progresses to a greater level of inflammation, causing diffuse alveolar damage and ultimately acute respiratory distress syndrome (ARDS), which is found to affect between 17-29 % of COVID-19 patients [8]. This serious functional impairment of the lungs is seen on chest CT as areas of consolidation. As a result, the presence and nature of consolidation areas seen on CT imaging is another marker for determining the severity and progression of COVID-19.
With this case finding of cannon-ball appearance on CT imaging of COVID-19, it adds yet another avenue to the unique presentations of COVID-19, necessitating distinguishing it from other forms of viral pneumonia. Cannon-ball appearance primarily signifies malignancy and sometimes other infectious diseases such as pulmonary tuberculosis, histoplasmosis, or cryptococcosis. Because COVID-19 is not notorious for cannon-ball appearance, pulmonary isolation may be delayed, potentially endangering medical personnel to exposure. COVID-19 becomes a diagnosis of exclusion for centers lacking testing since it is possible to rule out the other causes. Nonetheless, further data and studies are needed to fully understand this finding and to recognize it as a valid radiological sign for COVID-19.
Acknowledgment: No acknowledgments nor contributing authors to declare besides the ones stated.
Statement of Ethics: No human or animal subjects were harmed in the process.
Disclosure Statement: The authors have no conflicts of interest to declare.
Funding Sources: No funding sources to disclose.
Statement of Ethics
Published research complies with guidelines for human studies and animal welfare regulations. The patient has given informed consent and the institute’s committee for research approves of using the case for publication. There were no animals involved in the case report.
Author Contributions
Taha Sheikh, Praful Tewari, Ragheb Assaly were involved in the conception and design of the work.
Taha Sheikh, Luke Tsai, and Shamis Hasan were involved in manuscript writing.
Taha Sheikh and Ragheb Assaly were involved in reviewing and revising the manuscript.
Reference
-
Statement on the Second Meeting of the International Health Regulations (2005) Emergency Committee Regarding the Outbreak of Novel Coronavirus (2019-NCoV)”. 2020
-
“COVID-19 Weekly Epidemiological Update” World Health Organization, 18 Oct. 2020
-
Bernheim A, Mei X, Huang M, Yang Y, Fayad ZA, et al. (2020) “Chest CT Findings in Coronavirus Disease-19 (COVID-19): Relationship to Duration of Infection.” Radiology 295(3).
-
Kucirka LM, Lauer SA, Laeyendecker O, Boon D, Lessler J. (2020) “Variation in False-Negative Rate of Reverse Transcriptase Polymerase Chain Reaction–Based SARS-CoV2Tests by Time Since Exposure.” Annals of Internal Medicine 173(4): 262-267.
-
Zhu J, Zhimei Z, Li H, Ji P, Pang J, et al. (2020) “CT Imaging Features of 4121 Patients with COVID‐19: A Meta‐analysis.” Journal of Medical Virology 92(7): 891-902.
-
Xie X, Zhong Z, Zhao W, Zheng C, Wang F, et al. (2020) “Chest CT for Typical 2019-NCoV Pneumonia: Relationship to Negative RT-PCR Testing.” Radiology 296(2).
-
Wan S, Li M, Ye Z, Yang C, Cai Q, et al. (2020) “CT Manifestations and Clinical Characteristics of 1115 Patients with Coronavirus Disease 2019 (COVID-19): A Systematic Review and Meta-Analysis.” Academic Radiology 27(7): 910- 921.
-
Kanne JP, Little BP, Chung JH, Elicker BM, Ketai LH. (2020) “Essentials for Radiologists on COVID-19: An Update. Radiology Scientific Expert Panel.” Radiology 296(2).
-
Kshatriya R, Patel V, Chaudhari S, Patel P, Prajapati D, et al. (2016) “Cannon Ball Appearance on Radiology in a Middle- Aged Diabetic Female.” Lung India 33(5): 562-568.
-
Pan Y, Guan H (2020) “Imaging Changes in Patients with 2019-NCov.” European Radiology 30(10223): 3612-3613.



