Benali Saad1, *, Benlghazi Abdelhamid1, The Hassani Moulay El Mehdi1,2, Babahabib Abdellah1,2 and Jaouad Kouach1,3
1Department of gynecology and obstetrics, Mohamed V Military Training Hospital, Rabat, Morocco
2University Moulay Abdellah, FES, Morocco
3University Mohamed V, Rabat, Morocco
*Corresponding author: Saad B, Department of gynecology and obstetrics, Mohamed V Military Training Hospital, Rabat, Morocco
Abstract
Appendiceal mucocele is rare, observed on 0.2 to 0.6 % of appendicectomy peaces. Average age is about 50 to 60 - year-old with female predominance. Causes of appendiceal mucocele are multiple. Histologically, lesions are limited to mucosa. Treatment is based on surgery by classical appendicectomy with eviction of cellular dissemination. Prognosis of benign cases is excellent after complete resection with 5 years survival of approximately 100 %.
We report the case of a 54-year-old woman, menopaused, presenting isolated chronical pelvic pain and after all investigations, the diagnosis was found during the intervention and histopathological examination had confirmed appendiceal mucocele.
Keywords: appendiceal mucocele; ovarian tumor; histopathological diagnosis; clinical similarities; surgical treatment
Introduction
Appendiceal mucocele is a rare entity that is characterized by cystic dilatation in the lumen of the appendix. The diagnosis is often made based on clinical signs and symptoms of acute appendicitis or coincidentally via imaging methods when it is asymptomatic. However, it may rarely receive a definitive diagnosis before surgery despite all technical possibilities, and it may be encountered during abdominal surgery performed for another indication.
Observation
A 54-year-old woman, menopaused, presented to gynecological department for isolated chronical pelvic pain. Gynecological examination revealed latero-uterin mass, ferm, movable and well limited. Vaginal ultrasonography revealed heterogeneous mass measuring about 60 mm with both solid and cystic components, without suspicious vascularity at color Doppler. The MRI revealed suspicious loading vegetations within the mass (Figures 1-2).
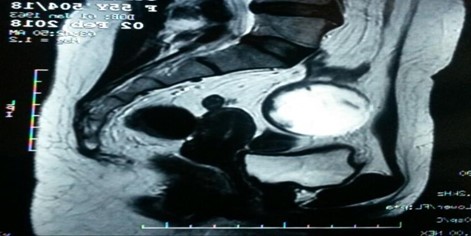
Figure 1: Sagittal MRI showing hyperintense rounded mass with vegetations
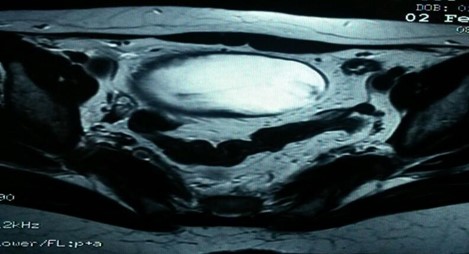
Figure 2: Transversal MRI showing hyperintense rounded mass
The patient has undergone diagnostic laparoscopy revealing an appendiculus mass measuring 12cm of the major axe. Surgical intervention has been converted to laparotomy with appendicectomy (Figures 3-4).

Figure 3: Macroscopic aspect of appendiculus mass

Figure 4: Macroscopic aspect showing the size of the mass
Histopathological examination revealed morphological aspect of appendicular mucinous adenoma.
Discussion
Appendiceal mucocele is a descriptive term referring to distention of the appendix with mucus, which develops secondary to mucinous cystadenoma (63 %), mucosal hyperplasia (25 %), mucinous cystadenocarcinoma (11 %) and retention cysts (1 %) of the appendix lumen [1]. Mucocele may also develop when the lumen is obstructed due to endometriosis or carcinoid tumors.
It is reported that the incidence of appendiceal mucocele in appendectomy specimens is 0.2 - 0.3 % [2]. Patients are generally above the age of 50, and it is 4 times more common among women [3]. Approximately 25-30 % of the patients are symptomatic, and it is incidentally identified during radiological studies, endoscopic examinations, or surgery [2,4]. The most frequent manifestation among patients with symptomatic appendiceal mucocele is acute or chronic lower right quadrant pain [3].
The mass may be palpated in the lower right quadrant in approximately half of the patients [5]. Other symptoms include nausea, vomiting and change in bowel habits [6]. It is difficult to correctly diagnose appendiceal mucocele before surgery due to non- specific symptoms [7]. Ultrasonography (US) and computerized tomography may aid in diagnosis. It is generally hypoechogenic in US; however, echogenicity may also be seen depending on the number of acoustic interfaces caused by the mucus. The onion skin- like appearance is specific for appendiceal mucocele [8]. Computerized tomography (CT) is more sensitive in recognizing and assessing appendiceal mucoceles. In CT, it is observed in the form of a cystic, encapsulated mass with a thin wall, which sometimes has mural calcifications, in the localization of the appendix [9].
There may be synchronous neoplasms with the appendiceal mucocele [10,11]. The most frequent synchronous neoplasm is that of the colon, however, it may also be present in other localizations such as gall bladder, breast, kidney, ovary and thyroid. In 19.4%–25.4% of the cases, appendiceal mucocele was found to be associated with colon adenocarcinoma [10]. For that reason, cases identified to have appendiceal mucocele should be assessed carefully with regards to colon neoplasms.
The treatment for appendiceal mucocele is surgery. Surgery may be performed via laparoscopy or laparotomy. It is important to be aware of the mucocele pre-operatively, and to avoid any manipulations during surgery, which may result in cystic rupture or leakage of the cystic fluid, because a potential rupture during surgery may cause pseudomyxoma peritonei. The 5-year survival rate with pseudomyxoma peritonei due to mucinous cystoadenocarcinoma may be as low as 20% [12]. Therefore, there are some publications which oppose the use of laparoscopy in surgery for mucocele, while there are other publications emphasizing that laparoscopic surgery can be successfully performed [13,14]. The reported case results and literature indicate that there are no contraindications for laparoscopic surgery in appendiceal mucocele. However, caution should be exercised to prevent its rupture during laparoscopy [14,15].
Conclusion
Appendiceal mucocele is a rather rare entity and it does not have a specific clinical presentation. Therefore, it is not considered as part of the differential diagnosis of lower right quadrant pain, and it is difficult to reach a pre-operative diagnosis. Appendiceal mucocele should be considered especially in cases where an elderly woman is observed to have a mass with atypical appearance in US or a mass is identified in the right iliac fossa. For this group of patients, laparoscopic excision performed with care following diagnostic laparoscopy may be a good option. Mucocele may often be associated with a concomitant colon cancer. Surgeons should always remember this and follow-up the patient.
References
- Bartlett C, Manoharan M, Jackson A (2007) Mucocele of the appendix-a diagnostic dilemma: a case report. J Med Case Rep 1: 183.
- Dachman AH, Lichtenstein LE, Friedman AC (1985) Mucocele of the appendix and pseudomyxoma peritonei. Am J Roentgenol 144(5): 923-929.
- Minni F, Petrella M, Morganti A, Santini D (2001) Giant mucocele of the appendix. Dis Colon Rectum 44: 1034-1036.
- Soweid AM, Clarkston WK, Andrus CH, Jannet CG (1998) Diagnosis and management of appendiceal mucoceles. Dig Dis 16(3): 183-186.
- Coulier B, Pestieau S, Hamels J, Lefebvre Y (2001) US and CT diagnosis of complete cecocolic intussusception caused by an appendiceal mucocele. Eur Radiol 12: 324-328.
- Carr NJ, McCarthy WF, Sobin LH (1995) Epithelial non carcinoid tumors and tumor-like lesions of the appendix. A clinicopathologic study of 184 patients with a multivariate analysis of prognostic factors. Cancer 75(3): 757-768.
- Shukunami K, Kaneshima M, Kotsuji F (2000) Preoperative diagnosis and radiographic findings of a freely movable mucocele of the vermi-form appendix. Can Assoc Radiol J 51(5): 281-282.
- Caspi B, Cassif E, Auslender R, Herman A, Hagay Z, Appelman Z (2004) The onion skin sign: a specific sonographic marker of appendiceal mucocele. J Ultrasound Med 23(1): 117-121.
- Fujiwara T, Hizuta A, Iwagaki H, Matsuno T, Hamada M, et al. (1996) Appendiceal mucocele with concomitant colonic cancer. Report of two cases. Dis Colon Rectum 39(2): 232- 236.
- Pitiakoudis M, Tsaroucha AK, Mimidis K, Polychronidis A, Minopoulos G, et al. (2004) Mucocele of the appendix: a report of five cases. Tech Coloproctol 8(2): 109-112.
- Moreno SG, Shmookler BM, Sugarbaker PH (1998) Appendiceal mucocele. Contraindication to laparoscopic appendectomy. Surg Endosc 12(9): 1177-1179.
- Chiu CC, Wei PL, Huang MT, Wang W, Chen TC, et al. (2005) Laparoscopic resection of appendiceal mucinous cystadenoma. J Laparoendosc Adv Surg Tech A 15:325-328.
- Navarra G, Asopa V, Basaglia E, Jones M, Jiao LR, et al. (2003) Mucous cystadenoma of the appendix: is it safe to remove it by a laparoscopic approach? Surg Endosc 17(5): 833-834.
- Lau H, Yuen WK, Loong F, Lee F (2002) Laparoscopic resection of an appendiceal mucocele. Surg Laparosc Endosc Percutan Tech 12(5): 367-370.
- Göksoy E, Geçioğlu A (1990) Appendix mucocele: A case report. Cerrahpaşa Tıp Fak Derg 21: 129-132.



