Torres Johny1*, Torres Juan2
1Internist. (https://orcid.org/0000-0001-8775-9260).
2First Year Hematology Resident. (https://orcid.org/0000-0002-8450-6150).
*Corresponding Author: Torres Johny, Internist. (https://orcid.org/0000-0001-8775-9260).
Abstract
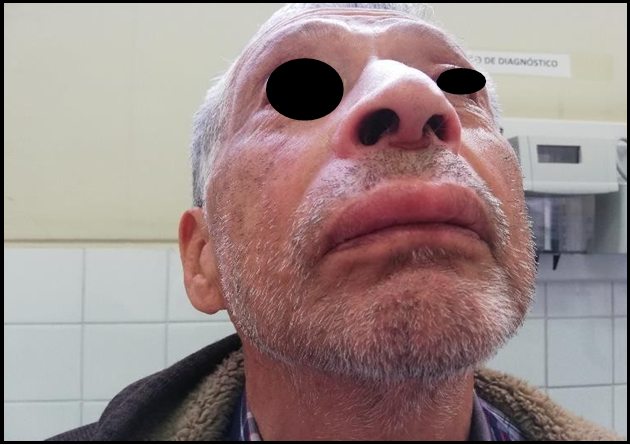
Angioedema is the swelling (usually localized), asymmetrical, and slightly painful that involves the face, lips, tongue, and swelling. Swelling can occur on the back of the hands, feet, and genitals and involves the deep dermis and subcutaneous cellular tissue due to increased vascular permeability in response to mediators derived from mast cells (histamine, leukotrienes, prostaglandins), bradykinin, and complement derivatives. We present the case of a 77-year-old male patient who, after endodontics in the upper dental arch, two days later presents outstanding edema of the upper lip and cheeks, which alarms him, and he goes again to the dental consultation where treatment based on corticosteroids and antihistamines is recommended, for 48 hours without improvement he goes for medical evaluation.
Physical examination: edematous facies, presence of significant edema of the upper lip and cheek, no involvement of the tongue, no skin color, no heat, no flushing, no inflammatory signs
Keywords: Angioedema, Angioneurotic edema, Labial edema, bradykinin, C1 inhibitor
Introduction
The first description of angioedema was made in 1882 by Heinrich I. Quincke. After Osler defined its hereditary character in 1888, acquired angioedema (AEA) was not identified until 1972. [1,2,3] Angioedema is the asymmetrical and slightly painful (usually localized) swelling involving the face, lips, tongue, and swelling on the back of the hands, feet, or genitals. It involves the deep dermis and subcutaneous cellular tissue due to increased vascular permeability in response to mast cell-derived mediators (histamine, leukotrienes, prostaglandins), causing urticaria and pruritus accompanying angioedema. At the same time, the one mediated by bradykinin and complement derivatives does not affect the dermis and does not present urticaria or pruritus. [8,4,5,6,7]
Its main clinical presentation is an asymmetrical and slightly painful swelling of the face, lips, and tongue, which may also be on the back of the hands, feet, or genitals, shocking to the patient and observer; the diagnosis is the physical examination. [3,6,7,8,9]
Occasionally, the intestine is involved with manifestations of obstruction: colic, nausea, vomiting.
Angioedema usually does not develop pruritus, urticaria, or bronchospasm, but sometimes laryngeal edema, stridor, and death. Urgent treatment is required when there is airway involvement.
Edema improves in 1 to 3 days in hereditary angioedema when the supplement is consumed and disappears without leaving sequelae.
It does not respond to antihistamines or corticosteroids; its treatment is for acute attacks with C1 inhibitors, Ecallantide, Icatibant, or lanadelumab, for attenuated androgen prophylaxis [9,10,11,12,13]
Case Presentation:
A 77-year-old married patient who makes baby clothes, with a personal history of Rheumatic Fever in his youth, treated with penicillin for more than 10 years, underwent a root canal 1 year ago. APF: mother diabetes, brother knee prosthesis. He went for endodontics in the upper dental arch without any problem. However, two days later, he presented outstanding edema of the upper lip and cheeks, which alarmed him, and he went again to the dental consultation, where they recommended treatment based on corticosteroids and antihistamines for 48 hours without improvement. He went for a medical evaluation
Physical Examination: BP: 100/60 HR: 104 RR: 18 saturation 93% BMI: 19.39 edematous facies presence of significant edema of the upper lip and cheek, no involvement of the tongue, skin color, no heat, no flushing no inflammatory signs
Laboratorio: proteínas totales 7.6g/dl, triglicéridos: 107mg/dl, ALT (SGPT):18u/l, AST(SGOT):21 u/l, glucosa: 94 mg/dl, Acido Urico: 5.6mg/dl, Urea: 37mg/dl Creatinine: 1.13 mg/dl, K: 4.71 mmol/l, Cl: 100 mmol/l, Na: 138mmol/l
Leukocytes: 92000 neutrophils 48%, lymphocytes 38%
TSH: 3,13Uui/ml, Testosterona: 9,77 ng/ml HIV: 0,12, PSA: 0,92
Definition:
Angioedema is the asymmetrical and slightly painful (usually localized) swelling involving the face, lips, tongue, and swelling on the back of the hands, feet, or genitals. Involves deep dermis and subcutaneous cellular tissue [1,3,5,11,12,13,14]
Epidemiology:
It is rare or infrequent because it is little known and underdiagnosed; it is estimated at 1 per-50,000 inhabitants, in Spain at 1.09 per- 150,000 inhabitants; the prevalence is unknown in our environment [2,5,8,13,14]
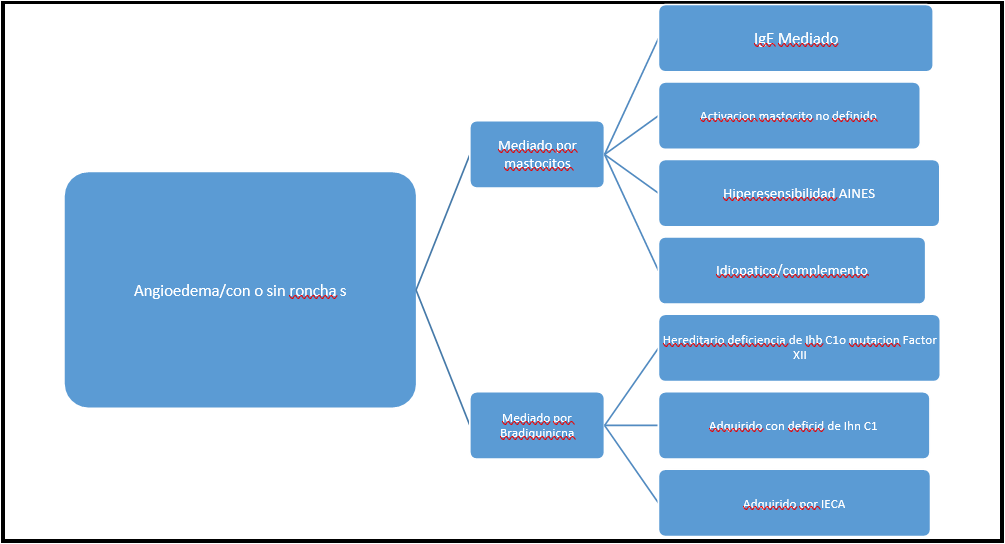
Classification:
There are currently 4 defined types of acquired angioedema and 7 types of hereditary angioedema [14,15,16]
Angioedema can be hereditary and acquired.
Hereditary Angioedema:
Inheritance is autosomal dominant of the SERPIG1 gene and manifests itself in childhood or adolescence, deficiency or dysfunction of complement inhibitor 1 (C1), it is a protein, its activity in the regulation of activation in the classical complement pathway, lecithin, kinin, coagulation and fibrinolytic activation; diagnosis is made by measuring C1complement inhibitor concentrations.
It also has 2 main types:
TYPE 1 (80 – 85%) its characteristic C1 inhibitor deficiency.
Type 2 (15-20%) is characterized by C1 inhibitor dysfunction. There is a rare type of hereditary angioedema listed as TYPE3 characteristic C1 inhibitor levels, prevalence is unknown, and occurs in women. (15,16,17,18)
Acquired Angioedema
It is even rarer and is related to other disorders, often being a consequence of autoimmune disorders such as the presence of anti- C1 inhibitor antibodies, lymphoproliferative diseases, in studies from the United Kingdom according to the frequency of chronic lymphocytic leukemia, non-Hodgkin's lymphoma, B-cell lymphoma, marginal zone lymphoma, follicular lymphoma, and Waldenstrom's macroglobulinemia (3,17,18)
Mechanism of C1 inhibitor deficiency
Supplement use in neoplastic disorders (e.g., B-cell lymphoma) or immune complex disorders.
Autoantibodies against C1 inhibitor in monoclonal gammopathies. Rarely are autoantibodies against C1 inhibitors generated in autoimmune diseases (e.g., lupus, dermatomyositis).
Triggers:
It is for all forms of angioedema, both hereditary and acquired: Minor trauma (e.g., dental repair, tongue piercing).
Viral illness. Exposure to cold Pregnancy
Ingestion of drugs or certain foods.
Angioedema is often aggravated by emotional stress
Aetiology:
The common mechanism is that C1 inhibitor deficiency or dysfunction affects complement activation and increases bradykinin concentrations by not blocking kallikrein activated in the synthesis pathway. [5,8,14,18]
Treatment: Treatment is proposed, for several moments, prophylaxis and acute crises [17,18,20]
Acute crises:
Ensuring the airway adrenaline can help, but corticosteroids and antihistamines don't work.
A human C1 inhibitor derived from purified plasma.
Ecalanthin (a recombinant protein that acts as a reversible kallikrein inhibitor). Icatibant (a synthetic decapeptide that acts as a reversible and competitive agonist of the type 2 kallikrein receptor) Lanadenumab (a recombinant monoclonal antibody that binds to plasma kallikrein and blocks its activity). Omalizumab 300 mg every 4 weeks for 6 months [13]
If none are available and the condition requires treatment, fresh frozen plasma, tranexamic acid, and alpha constant are also available. Rituximab, Methotrexate [19,20,21]
Long-term prophylaxis:
Attenuated androgens (e.g., Stanozol 2mg orally 3 times daily, danazol 200mg 3 times daily) stimulate hepatic production of C1 inhibitor, but are less effective for the acquired form.
Prophylaxis is indicated in the short term before risky procedures (e.g., dental or airway procedures) if a C1 inhibitor is not available; danazol and stanozolol are planned from 5 days before to 2 days after the operation.
If a C1 inhibitor is available, experts suggest using it 1 hour before high-risk procedures [19,20,21]
Evolution 5 Days
Acute Presentation
Discussion
As it is a rare pathology and is a response of mast cells to triggers (diet allergens, pollen, animal dander, dental resin, poisons, among others), in some cases, the cause is unknown, such as calcium antagonists, ACE inhibitors, muscle relaxants, fibrinolytic.
In our case, a reaction to the dental resin plus manipulation could have caused angioedema of the lip and face; according to his history, he does not use any medication. In addition, he does not have any intercurrent diseases. Angioedema was thought to be due to the characteristic location in the skin or mucosa of the face, and that has not improved with the use of corticosteroids and antihistamines; what was found in the patient was a state of anxiety due to his wife's illness in the last days with the risk of death, which could also be a trigger for the appearance of angioedema as reported in several studies, in the same way, the evolution towards the resolution of his edema in the following 72 hours without leaving any sequelae as reported in the literature.
As it does not respond to corticosteroids and antihistamines, there is no pruritus in the affected area, and there are no papules (hives), the mediator would be considered bradykinin or complement () due to the age of presentation it would be acquired angioedema or secondary to a lymphoproliferative or myeloproliferative disease that has not yet manifested. Therefore, the patient should be studied further to rule it out.
To confirm the diagnosis in our case, the determination of complement of C1 activity or the presence of a C1 inhibitor was not performed, as referred to in the literature to confirm the diagnosis.
References
- Aygören-Pürsün E, Magerl M, Maetzel A, Maurer M (2018) Epidemiology of Bradykinin-mediated angioedema: a systematic investigation of epidemiological studies. Orphanet J Rare Dis. 13(1): 73.
- Bork K, Machnig T, Wulff K, Witzke G, Prusty S, et al. (2020) Clinical features of genetically characterized types of hereditary angioedema with normal C1 inhibitor: a systematic review of qualitative evidence. Orphanet J Rare Dis. 15(1): 289.
- Ali HA, Lomholt AF, Mahmoudpour SH, Hermanrud T, Bygum A, von Buchwald C, et al. (2019) Genetic susceptibility to angiotensin-converting enzyme-inhibitor induced angioedema: A systematic review and evaluation of methodological approaches. PLoS One. 14(11): e0224858.
- Levy D, Craig T, Keith PK, Krishnarajah G, Beckerman R, et al. (2020) Co-occurrence between C1 esterase inhibitor deficiency and autoimmune disease: a systematic literature review. Allergy Asthma Clin Immunol. 16: 41.
- James C, Bernstein JA (2017) Current and future therapies for the treatment of histamine-induced angioedema. Expert Opin Pharmacother. 18(3): 253-262.
- Depetri F, Tedeschi A, Cugno M (2019) Angioedema and emergency medicine: From pathophysiology to diagnosis and treatment. Eur J Intern Med. 59: 8-13.
- Cicardi M, Suffritti C, Perego F, Caccia S (2016) Novelties in the Diagnosis and Treatment of Angioedema. J Investig Allergol Clin Immunol. 26(4): 212-21.
- Kaplan AP (2014) Bradykinin-mediated diseases. Chem Immunol Allergy. 100: 140-7.
- Kaplan AP, Joseph K (2014) Pathogenic mechanisms of bradykinin mediated diseases: dysregulation of an innate inflammatory pathway. Adv Immunol. 121: 41-89.
- Nowicki RJ, Grubska-Suchanek E, Porêbski G, Kowalski ML, Jahnz-Różyk K, et al. (2020) Angioedema. Interdisciplinary diagnostic and therapeutic recommendations of the Polish Dermatological Society (PTD) and Polish Society of Allergology (PTA). Dermatol Alergol advances. 37(4): 445-451.
- van den Elzen M, Go MFCL, Knulst AC, Blankestijn MA, van Os-Medendorp H, et al. (2018) Efficacy of Treatment of Non- hereditary Angioedema. Clin Rev Allergy Immunol. 54(3): 412- 431.
- Rosi-Schumacher M, Shah SJ, Craig T, Goyal N (2021) Clinical manifestations of hereditary angioedema and a systematic review of treatment options. Laryngoscope Investig Otolaryngol. 6(3): 394-403.
- Savarese L, Mormile I, Bova M, Petraroli A, Maiello A, et al. (2021) Psychology and hereditary angioedema: A systematic review. Allergy Asthma Proc. 42(1): e1-e7.
- Nicola S, Rolla G, Brussino L (2019) Breakthroughs in hereditary angioedema management: a systematic review of approved drugs and those under research. Drugs Context. 8: 212605.
- Kaegi C, Wuest B, Schreiner J, Steiner UC, Vultaggio A, et al. (2019) Systematic Review of Safety and Efficacy of Rituximab in Treating Immune-Mediated Disorders. Front Immunol. 10: 1990.
- Lewis LM (2013) Angioedema: etiology, pathophysiology, current and emerging therapies. J Emerg Med. 45(5): 789-96.
- Hofman ZLM, van West N, Hack CE, Knulst AC, Maas C, Röckmann H (2019) High occurrence of antihistamine resistance in patients with recurrent idiopathic angioedema. Clin Transl Allergy. 9: 35.
- Long BJ, Koyfman A, Gottlieb M (2019) Evaluation and Management of Angioedema in the Emergency Department. West J Emerg Med. 20(4): 587-600.
- Muller Y, Harr T (2016) Treatment of drugs-associated non- hereditary angioedema mediated by bradykinin. Rev Med Switzerland. 12(500): 11-2.
- Maurer M, Magerl M, Betschel S, Aberer W, Ansotegui IJ, et al. (2022) The international WAO/EAACI guideline for the management of hereditary angioedema - The 2021 revision and update. World Allergy Organ J. 15(3): 100627.
- Blaiss MS, Bernstein JA, Kessler A, Pines JM, Camargo CA et al. (2022) The Role of Cetirizine in the Changing Landscape of IV Antihistamines: A Narrative Review. Adv Ther. 39(1): 178-192.