Namrah Khalid*, Laiba Masood, Aiman Mahmood
Shifa International Hospital, Islamabad, Pakistan
*Corresponding Author: Namrah Khalid, Shifa International Hospital, Islamabad, Pakistan
Abstract
A rare but potentially fatal complication of a leiomyoma is a suppurative leiomyoma or pyomyoma, resulting from infarction and infection. Our case involved a pyomyoma secondary to a lesser-known cause of uterine artery embolization. Owing to its nonspecific presentation and infrequent occurrence, a high index of clinical concern is critical in diagnosis. Clinical symptoms in combination with multimodality imaging, help in the accurate diagnosis and time accurate management of patient.
Keywords: Pyomyoma; Uterine artery embolization; Abdominal sepsis.
Introduction
A rare but potentially fatal complication of a leiomyoma is a suppurative leiomyoma or pyomyoma, resulting from infarction and infection. The incidence is unknown, but it was previously estimated to be under 1% of operated fibroids, [1] and approximately 100 cases have been reported since 1945. Owing to low clinical suspicion, diagnosis is often delayed, resulting in possible complications such as sepsis or purulent peritonitis.
Uterine artery embolization (UAE) is a non-invasive procedure that is increasingly used for symptomatic fibroids and is a very rare complication of pyomyoma. We present a similar rare complication of pyomyoma after UAE and subsequent discussion of the literature.
Case Presentation
Our patient is a 36-year-old nullipara female, who has been married for seven months. She initially experienced symptoms of lower abdominal heaviness and presented to the outside facility with symptoms of heavy vaginal bleeding with clots and dysmenorrhea. She underwent an MRI of the pelvis with contrast. The report revealed a large pedunculated subserosal fibroid along the anterior uterine wall displacing the uterus posteriorly, measuring 7.6 x 10 x 11 cm. Owing to her symptoms, she was scheduled for uterine artery embolization. The procedure details included 3D processing of the pelvic vasculature for super selective embolization of the bilateral uterine arteries. Selective catheterization was performed to embolize the distal segment of the bilateral uterine arteries. Bilateral intra-arterial treatment for postembolization syndrome, as well as bilateral intra- arterial pain management for post embolization pain, was performed. A successful fluoroscopic-guided superior hypogastric nerve plexus block was performed for extended pain relief. Embolization was performed with FDA-approved 500 - 700 microns and 700 - 900 microns medical particles/devices. The catheter and sheath were removed, and hemostasis was achieved. The patient tolerated the procedure well.
After one month, she presented to the emergency department of our hospital with complaints of severe abdominal pain and fever. She underwent a detailed laboratory investigation. [Table 1]
|
Tests |
Results |
Normal Ranges |
|
WBC total |
38220/uL |
(4000-10000) /uL |
|
RBC total |
5.24m/uL |
(3.8-4.80) m/uL |
|
Hemoglobin |
9.8 g/dl |
(12-15) g/dl |
|
HCT |
31% |
(36-46.0) % |
|
MCV |
60.5 fL |
(83.0-101.0)fL |
|
MCH |
18.7 pg |
(27.0-32.0)pg |
|
MCHC |
30.9 g/dL |
(31.5-34.5)g/dl |
|
Platelets |
641000 /uL |
(150,000-450,000)/uL |
|
Neutophils |
81% |
(40-80)% |
|
lymphocytes |
10% |
(20-40)% |
|
RDW |
15.20% |
(11.6-14.0)% |
|
CRP |
376 mg/L |
upto 5.0mg/L |
|
Lipase serum |
27 U/L |
13-60 U/L |
|
AST |
18 U/L |
upto 35 U/L |
|
ALT |
10 U/L |
upto 35 U/L |
|
ALP |
73 U/L |
40 -130 U/L |
|
Bilirubin |
0.74 mg/dl |
upto 1.2 mg/dl |
|
Gamma G.T |
39 U/L |
upto 40 U/L |
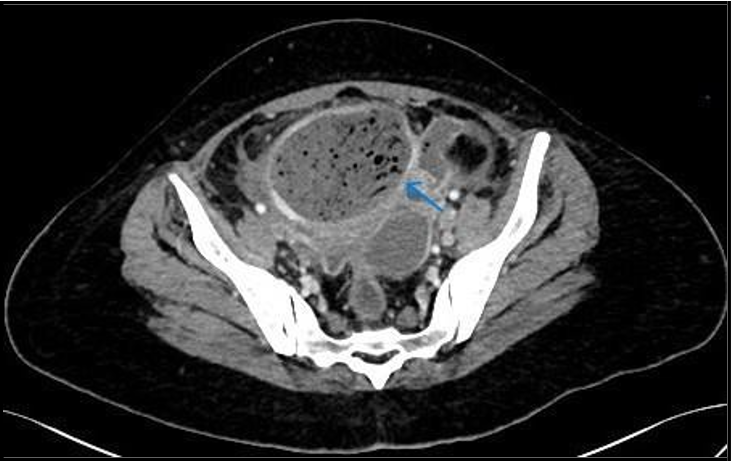
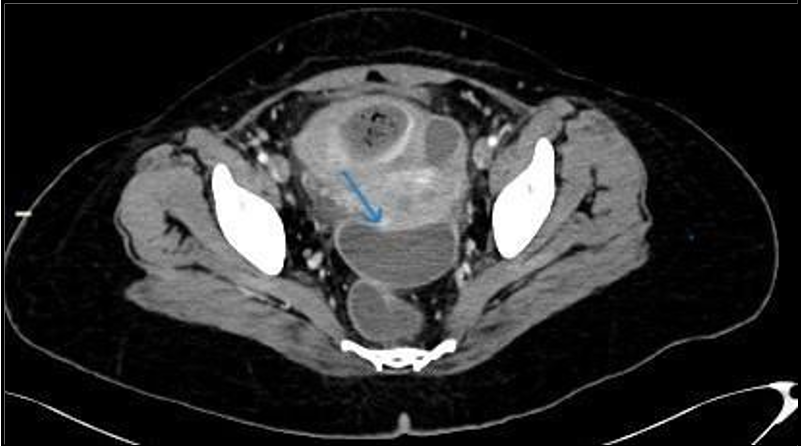
A CT scan of the abdomen and pelvis with contrast was performed to determine the cause of sepsis. It revealed a large, thick, enhancing walled-off area in the pelvis adjacent to the fundus of the uterus, containing multiple internal air locules with indistinct walls at places, and continuing air tracks. (Figure 1, 2). This represented an infected embolectomy-treated subserosal fibroid. There were multiple intercommunicating pelvic infection collections in the cul-de-sac and vesico-uterine pouch (Figure 3). Diffuse peritonitis, omentomesenteric congestion, and edematous bowel loops were observed. Multiple prominent pelvic sidewall nodes were also noted. Therefore, rupture of pyomyoma with intraperitoneal spillage of infected content resulting in peritonitis is suggested.
Figure 1: Axial images of contrast enhanced CT scan showing air containing mid pelvic structure/pyomyoma (arrow).
Figure 2: Coronal images of contrast enhanced CT scan showing diffuse peritoneal reaction and fluid.
Figure 3: Pelvic abscesses with larger in Cul de sac (arrow).
The patient was admitted under surgical services and underwent diagnostic laparoscopy. Once the abdomen was entered, extensive adhesions were noted, so the procedure was converted to open laparotomy. Intraoperative findings included pus in all of the abdominal quadrants and interloop pus. The subserosal fibroid was identified and removed. The fundus of the uterus was torn, which was then repaired intraoperatively, and hemostasis was secured. Afterwards, the peritoneal wash was performed thoroughly, and a pelvic drain was placed. Postoperatively, the patient had an uneventful hospital stay.
A large biopsy sample of uterine fibroid myomectomy revealed infarction and hyalinization and was negative for malignancy. A microscopic description revealed a benign smooth muscle tumour showing extensive infarct-type necrosis with viable areas identified at the periphery; the tumour was composed of spindle-shaped cells with cigar-shaped nuclei and eosinophilic cytoplasm. The infarcted areas show ghostly outlines of smooth muscle fibres. Immunohistochemistry was positive for ASMA. Pus C/S moderately promoted the growth of Enterobacter species. The patient was discharged on minocycline- HCL and Flagyl tablets.
Discussion
Leiomyomas or fibroids are the most common gynecological and uterine benign smooth muscle neoplasms, which are hormone dependent, and typically develop after menarche and regress after menopause. The lifetime prevalence usually exceeds 70% in women.[2] They are most found within the myometrium, but they can also be seen in the broad ligament, cervix, or ovaries. Most patients are asymptomatic (approximately 50%). Nevertheless, they can present with acute or chronic symptoms, including menstrual disorders, pain, subfertility, and symptoms secondary to mass effects on the urinary bladder or bowel. They can rapidly increase in size during pregnancy, with increased chances of red degeneration due to hemorrhagic infarction. Other types of degeneration encountered are hyaline, cystic, or mixed. Clinical management mainly aims to reduce the symptoms and increase the chances of fertility with medical and interventional options.
Pyomyoma is a rare complication of a fibroid that can be observed in the postpartum period, pregnancy, cesarean section, or uterine instrumentation procedures, such as dilation and curettage, and can provide a direct source of inoculation of infective pathogens, accounting for a significant number of reported cases. [3, 4] Additional factors, including diabetes, immunocompromised conditions, hypertension, IV drug use, the presence of intrauterine devices, submucosal leiomyomas, preexisting infections, and advanced age, are increasingly associated with the development of pyomyoma. [5]
The exact etiology behind pyomyoma is uncertain; however, theories suggest that vascular compromise is a prime factor resulting in uterine fibroid necrosis and thus an environment suitable for infection. [6] The roots of infection are typically contiguously spread from the endometrial cavity, hematogenous/lymphatic spread, or direct extension from adjacent adnexa or bowel. Pyomyomas can extend deep into the myometrium or may penetrate or rupture into the abdomen, abdominal wall, surrounding pelvic organs, or the endometrial cavity.
Uterine artery embolization is an endovascular noninvasive procedure with the basic goal of causing necrosis and ischemia of the fibroid to help achieve a reduction in size. This method has been widely used for symptomatic patients, with a reduction in bulk symptoms of 77% after six months, an average decrease in uterine size of 48%, and approximately 85% control of menorrhagia after six months. [7] Despite the strong evidence of the efficacy and safety of UAE procedures and lower complication rates than surgical procedures, UAE is currently a much more widely used procedure. Pyomyoma is a unique and rare complication of UAE that should also be considered. Approximately 13 cases of pyomyoma have been reported to be secondary to UAE since 1945 in patients aged 28--65 years, and approximately all of them were larger than 7 cm. [8-10] Pyomyomas measuring up to 13 cm have also been reported to develop secondary to UAE. [4] Patients usually present with fever, pain, and leukocytosis, as was the case with our patient. The amount of embolic material or the type used is not usually considered a risk factor for pyomyoma. [11] The period for presentation after UAE is usually 6--56 days, with our patient presenting at approximately the 40th day post-procedure.
The cross-sectional imaging appearance usually reveals an enlarged uterus containing a fibroid with necrosis and multiple gaseous foci. The diagnosis can be difficult because of the often-insidious onset of presentation and the rarity of this condition. The triad of a fibroid, sepsis, and an unknown source of infection should raise clinical concerns about pyomyoma. [12] Other symptoms can include vaginal discharge, bleeding, fever and abdominal pain. The blood workup usually reveals leukocytosis, with a literature review showing that 57 out of 70 patients had leukocytosis greater than 11,000 cells/uL. However, positive cultures are not always obtained, with similar studies showing positive cultures in only 21 of 63 cases. [13] However, cultures obtained from pyomyoma are often positive (seen in 54 out of 61 cases), with the most common organisms being Staphylococcus species, E. coli, streptococcal species, enterococcal species, and a few cases of Proteus mirabilis. [4, 13]
One differential condition for postembolization leukocytosis, fever, and abdominal pain is postembolization syndrome (PES). Approximately 86% of the patients after UAE have mild leukocytosis, with approximately 21% of patients showing clinically elevated levels. [10] High-grade leukocytosis, foul-smelling vaginal discharge, and presentation one week after the procedure, along with symptomatic responsiveness to antibiotics, favor infectious processes such as pyomyoma.
The imaging modalities used for the diagnosis of pyomyomas are generally ultrasound, CT, and MRI. Ultrasound may reveal a sizable uterus containing a heterogeneous echogenic mass showing acoustic shadowing because of gas. Abulafia et al.in 2010, suggested that on ultrasound, the presence of normal myometrium in the form of an anechoic halo outlining the mass can be highly suggestive or even pathognomic for pyomyoma. [15] A heterogeneous mass with cystic components, necrotic debris, gas, and a peripheral enhancing rim are CT appearances, [10] as in our case.
Ruptured pyomyoma can present with abdominal sepsis, and free intraperitoneal air with infective collections/abscesses in the abdomen. On MRI, diffusion weighted imaging (DWI) is useful for identifying abscesses and performing biopsies for diagnosis before surgery. [14] On imaging, the differential diagnosis for pyomyoma can include gynecological tumors of ovarian or tubo-ovarian origin, endometriosis, appendiceal mucocele, or gastrointestinal stromal tumors. Red degeneration is also an important entity due to its similarity to a pyomyoma.
Since the advent of intravenous antibiotics, mortality secondary to pyomyoma has significantly decreased from 33-70% to <2% since 1990. [13] Empiric antibiotic regimens include covering gram- negative organisms and anaerobes. The definitive treatment is surgical intervention, with procedures ranging from minimalist intervention, such as drainage of the abscess, to hysterectomy, all of which are contingent on the extent and severity of the disease. In accordance with patient preferences, uterus-preserving surgeries with myomectomy can also be considered and have been successful. [8, 9] Image-guided percutaneous drainage of abscesses can provide temporary relief and control of infection in cases where surgical intervention is not immediately feasible. The required management plan largely depends on a multitude of factors, including the clinical condition of the patient, the extent of the disease, consideration of fertility, and available expertise at the healthcare facility. A multidisciplinary approach including radiologists, gynecologists, infectious disease specialists, and surgeons is needed to provide comprehensive care to patients and achieve feasible outcomes.
Conclusion
Owing to its nonspecific presentation and rare occurrence, a high index of clinical concern is critical in the diagnosis of pyomyoma. Clinical symptoms in combination with multimodality imaging, help in the accurate diagnosis and timely management of patients.
Abbreviations
UAE- Uterine artery embolization
ASMA - Anti-Smooth Muscle Antibody
FDA- Food and Drug Administration
CT - Computed Tomography
MRI - Magnetic Resonance Imaging
PES- post-embolization syndrome
Fundings: None to declare.
Submission Statement: This submission has not been previously published or in under consideration for publication in any journal.
Ethical Statement: IRB approved as per the ethical guidelines of hospital board. Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in- Chief of this journal on request.
Credit Authorship Contribution Statement:
NK: Writing – original draft.
LM: Writing – review & editing.
AM: Conceptualization.
Declaration Of Competing Interest: All authors declare no conflict of interest.
Data Availability: The data that has been used is confidential.
References
- Miller I (1945) Suppurating fibromyomas: report of a case with a review of the literature. Am. J.Obstet.Gynecol. 50(5): 522-6.
- Baird DD, Dunson DB, Hill MC, Cousins D, Schectman JM (2003) High cumulative incidence of uterine leiomyoma in black and white women: ultrasound evidence. Am. J. Obstet. Gynecol.188(1): 100-7.
- Iwahashi N, Mabuchi Y, Shiro M, Yagi S, Minami S et al.(2016) Large uterine pyomyoma in a perimenopausal female: A case report and review of 50 reported cases in the literature. Mol. Clin. Oncol. 5(5): 527-31.
- Bechay K, Thomas M, Le T BR, Vuu K, Quinn B (2022) Large pyomyoma after an urgent uterine artery embolization (UAE). J. Clin. Images Med. Case Rep. 3(10): 2128.
- Vulasala SS, Gopireddy DR, Mohamed K, Lall C (2021) Ruptured pyomyoma–rare complication of post-uterine artery embolization: a case report. J. Clin. Imaging Sci. 11(1): 67.
- Wynn AB, Shultz RL, Dayton EF, Farmer K (2024) Prolapse of a large degenerating uterine leiomyoma: a case report. Cureus. 16(5): 60622.
- Hutchins Jr FL, Worthington-Kirsch R, Berkowitz RP (1999) Selective uterine artery embolization as primary treatment for symptomatic leiomyomata uteri. J. Am. Assoc. Gynecol. Laparosc. 6(3): 279-84.
- Yu Q, Gabriel G, Hoffman M, Sanampudi S, Jassim T et al. (2019) Uterine-sparing management of pyomyoma after uterine fibroid embolization. Radiol. Case Rep. 14(8): 1031-5.
- Busshoff J, Thangarajah F, Morgenstern B (2022) Uterus- preserving management of Pyomyoma: case report of a rare complication after uterine artery Embolization. Case Rep. Women Health. 34: 00405.
- Ezzedine D, Ndubizu C, Kayani S, David A (2020) Pyomyoma after uterine artery embolization: A case report. Case Rep. Women Health. 26(1): 00186.
- Obele CC, Dunham S, Bennett G, Pagan J, Sung LY, et al. (2016) A case of pyomyoma following uterine fibroid embolization and a review of the literature. Case Rep. Obstet. Gynecol. 1: 9835412.
- Greenspoon JS, Ault M, James BA, Kaplan L (1990) Pyomyoma associated with polymicrobial bacteremia and fatal septic shock: case report and review of the literature. Obstet. Gynecol. Surv. 45(9): 563-9.
- Azimi-Ghomi O, Gradon J (2017) Pyomyoma: case report and comprehensive literature review of 75 cases since 1945. SM J Case Rep. 3(4): 1054.
- Peris H, Del Riego J, Criado E, García-Chamón RB, Vall E et al. (2022) Value of diffusion-weighted magnetic resonance imaging in the diagnosis of pyomyoma. Radiol. Case Rep. 17(1): 137-41.
- Abulafia O, Shah T, Salame G, Miller MJ, Serur E, et al. (2010) Sonographic features associated with post–uterine artery embolization pyomyomaj. Ultrasound Med. 29(5): 839-42.