Safaa Choayb*, Kaoutar Imrani, Nabil Moatassim Billah, Ittimade Nassar
Radiology Department, Ibn Sina University Hospital, Rabat, Morocco
*Corresponding Author: Safaa Choayb, Radiology Department, Ibn Sina University Hospital, Rabat, Morocco.
Abstract
Splenosis is a benign acquired condition characterized by autotransplantation of splenic tissue in the peritoneal cavity in patients with a history of traumatic splenic injury and splenectomy. We present the case of a 35 years-old patient with a history of resected breast cancer who presented for a follow-up examination. CT scan revealed multiple sclerosis nodules in the peritoneal cavity mimicking peritoneal metastasis.
Keywords: Abdominal splenosis, splenosis, peritoneal sclerosis.
Case Presentation
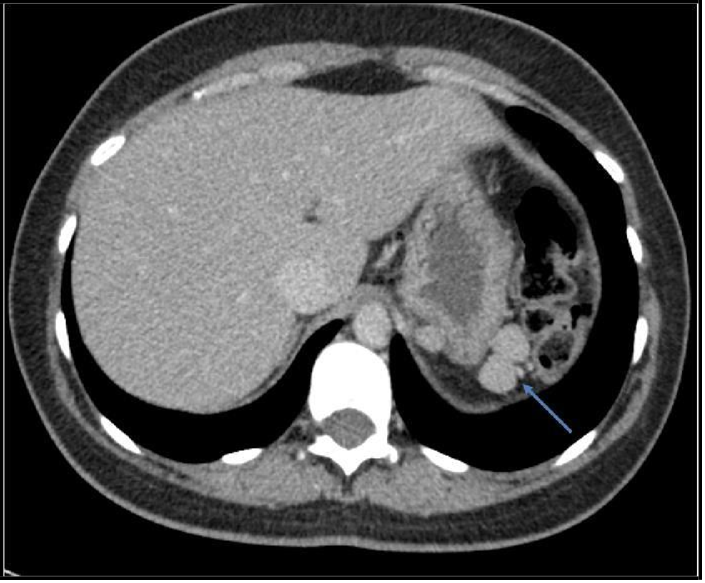
We present the case of a 35 years-old patient with a history of resected breast cancer presented for a follow-up CT examination. Abdominal imaging revealed multiple solid nodules in the peritoneal cavity, particularly in the left upper quadrant showing homogenous enhancement at the portal phase.
Peritoneal carcinomatosis was suspected at first. Biopsy was in favor of splenosis nodules.
The re-interrogation revealed a history of closed abdominal trauma at the age of 10.
Figure 1: CT scan of the abdomen and pelvis. Axial slice. Nodular lesions of round morphology, with soft tissue density and enhancement with the contrast medium in the left upper quadrant
Figure 2: CT scan of the abdomen and pelvis. Axial slice. Nodular lesions of round morphology, with soft tissue density and enhancement with the contrast medium in the right iliac fossa.
Discussion
Splenosis is a benign acquired condition secondary to auto-transplantation of splenic tissue in other organs or within cavities or thorax after prior splenic trauma or surgery. The true incidence of this condition is unknown because it is usually an incidental finding. However, splenosis has been reported in up to 67 % of patients with a history of splenic trauma [1].
It is more commonly detected in males, which may be due to the higher incidence of trauma in young men. Less naturally, spontaneous non-traumatic rupture of the spleen can occur in newborns due to severe hemolytic disease and secondary to infectious mononucleosis in older children and teenagers [2].
The name ‘splenosis’ was proposed by Buchbinder and Lipkoff in 1939 to describe the heterotopic transplantation of splenic tissue secondary to splenic trauma or surgery. However, the first description appeared much earlier. In 1883, Griffin and Tizzani noticed splenosis in dogs. The first human cases were recorded only in 1896 by Albrecht and in 1907 by Schilling.
The mean time between spleen injury and the diagnosis of splenosis differs from 5 months to 32 years (an average of 10 years) [3].
The beginning of the seeding process is presumed to be secondary to the spillage of the damaged splenic pulp into the adjacent cavities or by hematological spread to distant organs.[4] This mechanism explains the finding of hepatic and intracranial stenosis foci [5].
The peritoneal cavity is the most common implantation site of splenosis, with the left hypochondriac region being the most common location [1]. Other common areas include the small intestine serosa, greater omentum, parietal peritoneum, large intestine serosa, mesentery, and under the surface of the diaphragm. The implants can be solitary or multiple. Their number can range from a couple to up to 400 nodules, and the size of these nodules varies from a few millimeters to 12 cm. However, nodules rarely become more significant than 3 cm due to their local blood supply constraints, which limit their growth [6].
Peritoneal sclerosis must be distinguished from congenital variations of the spleen, including accessory spleen and polysplenia syndrome. Accessory spleens are congenital, arising from the dorsal mesogastrium during the embryonic period, usually solitary, located near the spleen, in the region of gastrosplenic ligaments, and receiving blood supply from the splenic artery. Histologically these resemble the normal spleen with a hilus, normal pulp, and splenic capsule [4]. Polysplenia with situs ambiguous, also known as bilateral left-sidedness or left isomerism, is a congenital syndrome more common in females associated with multiple highly variable visceral and cardiovascular anomalies [2].
Splenosis may mimic malignancies, including carcinomatosis, liver tumor, metastatic right adrenal mass, lymphoma, primary neoplasms, peritoneal mesothelioma, gliomatosis peritonei, granulomatous peritonitis, and lung cancer [1][7].
The majority of patients with stenosis are asymptomatic. In symptomatic cases, abdominal pain is the most frequent manifestation, secondary to infarction and bleeding of the implants, peritoneal adhesions, and intestinal obstruction. The specific locations of the implants can generate less frequent symptoms. For example, gastrointestinal tract hemorrhage has been reported by foci in the gastrointestinal tract and hydronephrosis due to extrinsic compression of the ureters.
The diagnosis of the entity, in general, is incidental and is related to evidence of splenic implants in imaging studies or during surgical procedures. Ultrasound shows nodules or round abdominal masses, with well-demarcated contours and solid appearance, hypo- to isoechoic in the center, with an incomplete hyperechoic ridge and posterior acoustic reinforcement [1][5]. If Doppler can be used, the absence of a central artery and the presence of vessels penetrating the capsule allow differentiation with accessory spleens [5].
CT allows for a precise number, size, and morphology of the nodules, which show density and enhancement similar to the spleen. In the case of hepatic splenosis, the nodules are a low signal after the administration of contrast medium, a high alert in the arterial phase, a medium signal in the portal phase, and a joint call in the equilibrium phase [5]. On MRI, they demonstrate intermediate to low signal intensity on T1-weighted images, medium to high signal intensity on T2-weighted images, and restricted diffusion, with signal characteristics and an enhancement pattern of normal splenic tissue [2].
Spleen implants remain functional, which can have positive and negative involvements. A disadvantageous consequence is the possibility of recurrence of the disease that was the cause of the previous splenectomy. On the positive side, this might reduce the risk of serious infections caused by capsular bacteria, including sepsis [3]. Pathologic analysis is considered the gold standard for diagnosing stenosis, but it is an invasive procedure that is not immune to complications. Therefore, scintigraphy with Tc99m-labelled heat-denatured red blood cells (Tc-99m-DRBC) is nowadays preferred for the definitive diagnosis, capable of proving splenic tissue.[1].
In our case, the patient had a history of breast cancer, and histology was necessary to rule out the diagnosis of peritoneal carcinomatosis, even with a history of abdominal trauma.
Conflict of Interests: The authors declare that there is no conflict of interest regarding the publication of this paper.
Author Contributions: All authors contributed equally to this work
References
- Vernuccio F, Dimarco M, Porrello G, Cannella R, Cusmà S, et al. (2021) Abdominal splenosis and its differential diagnoses: What the radiologist needs to know. Curr Probl Diagn Radiol. 50(2): 229-235.
- Tandon YK, Coppa CP, Purysko AS (2018) Splenosis: a great mimicker of neoplastic disease. Abdom Radiol (NY). 43(11): 3054-3059.
- Chorbińska J, Krajewski W, Sroczyński M, Guziński M, Zdrojowy R (2020) Splenosis mimicking lymphadenopathy. Journal of Surgical Case Reports. 2020(10): rjaa425.
- Vergara D, Ginolfi F, Moscati S, Giordano B, Ferrara N, et al. (2018) Multiple intra-hepatic and abdominal splenosis: an easy call if you know about it. Acta Radiol Open. 7(5): 2058460118772324.
- Alberto J, Bayona C (2017) Abdominopelvic Splenosis: Case Report and Literature Review. Rev. Colomb. Radiol. 28(4): 4825- 7.
- Guzman Rojas P, Parikh J, Mahne A, Vishnubhotla P, Oharriz JJ (2018) Where is My Spleen? – A Case of Splenosis Diagnosed Years Later after Splenectomy. 10(5): e2618.
- Kosydar SR, Sanchirico PJ, Pfeiffer DC (2020) A case of thoracoabdominal splenosis. Radiology case reports. 15 (1): 7-10.