Ahmed Ali Alrizqi*, Musab Atif Alamri, Jaber Abdullwhab Asiri, Hussian Mohammed Alamri, Ahad Hamdan Saeed
Medical Imaging Department King Saud Medical City Ulaishah, Riyadh, Saudi Arabia
*Corresponding Author: Ahmed Ali Alrizqi. Medical Imaging Department King Saud Medical City Ulaishah, Riyadh, Saudi Arabia
Abstract
A complication of severe hemophilia when the regular factor activity in the human blood is below 1 % can cause hemophilic pseudotumor. Diagnosing HP can be challenging. Also, the difficulty arises from needing more patient history. Missing the patient’s history, such as not knowing the patient’s hemophilia, makes the diagnosis more demanding. This case report presents a rare case of abdominal hemophilic pseudotumor. MRI and CT scans can be handy tools to diagnose HP. Additionally, investigating the patient history due to the similarity between HP and another similar cyst, such as hydatid cysts, can also be helpful.
Introduction
A complication of severe hemophilia when the regular factor activity in the human blood is below 1 % can cause a hemophilic pseudotumor (HP). HP is an encapsulated gradually increasing hematoma in the soft tissue or the musculoskeletal system. The characteristics of HP are a large mass with blood clots; in some stages, this mass is covered by fibrous material. In the case of soft tissue, HP can be extra muscular or intramuscular. According to the case reports and the literature, most patients reported HP in the musculoskeletal system, and a few are found in the soft tissue or the abdominal cavity [1]. Commonly, mural nodules are seen in HP patients. Furthermore, abdominal HP can cause colonic obstruction, fistula to the skin or the large intestine, and compression of nerve vessels [2].
Computed tomography (CT) and magnetic resonance imaging (MRI) is ideal for diagnosing HP. However, HP appears in CT scans to evaluate the Hounsfield scale or Hounsfield Unit (HU); in most cases, the HU for HP is between (10-35 HU), and it contains calcification or is covered by fibrous material [3]. Still, HP appearance can be challengeable in CT with contrast because of the similarity of some other disorders, such as brown tumor chondroma and hydatid cyst [4] On the other hand, MRI shows T2 signal intensities corresponding to blood in several stages of evolution. When HP is surrounded by capsules T1 and T2, it appears with low signal intensity. It is clear on T2 weighted imaging [2].
Abdominal HP treatment has not been standardized because of rare cases; however, surgical, ultrasound-guided puncture, radiation therapy, and medications might be patient options. The surgical approach is more effective in sizeable hemophilic pseudotumors [5]. This case report presents a rare case of abdominal hemophilic pseudotumor.
Case Report
A 41-year-old man came to the emergency room at King Saud Medical City, complaining of severe abdominal pain with a history of hemophilia. A hard mass in the left lower quadrant and a hernia in the abdominal midline. The patient had this pain for 2-3 years before seeking treatment. The patient antihemophilic factor VIII was less than 1%. In addition, the patient does not own any pets or livestock. The first CT scan with contrast finding was a giant left abdomen complex lesion with an avidly enhancing wall with few calcified flecks. The lesion measured 16 x10 × 13 cm, containing fluid density and a dense eccentric nodule with multiple adjacent smaller cystic lesions on the anterior aspect. Also, a similar lesion is seen in the right psoas muscle. It shows internal septation with calcification and a thick enhancing wall. Other small cystic lesions are seen in the left anterior abdominal wall peritoneum. The CT report suggested an MRI scan with contrast for more characterization (Figure 1)
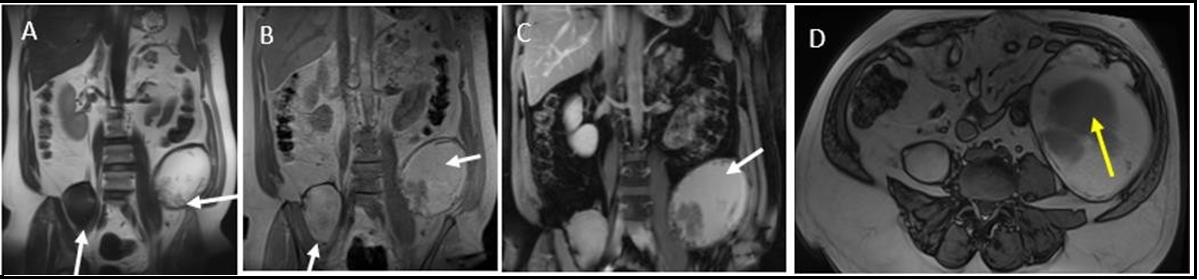
MRI reports a demonstration of the large irregular heterogeneous fluid-filled lesion in the left retroperitoneum and right psoas muscle. It shows central bright signal intensity in T1 and T2 weighted images with no enhancement in subtracted images, indicating a large hematoma. The lesion wall shows dark signal intensity in T2 weighted images representing fibrous. The internal lesion nodule with no enhancement is a blood clot (Figure 2)
The final impression was based on the patient history, and CT and MRI highly suggested hemophilic pseudotumor.
Figure 1: CT abdomen and pelvic with contrast (A) an axial view and (B) a coronal view. (A, B) Retroperitoneal complex cystic lesions seen in the left lower abdomen (horizontal white arrows), right psoas muscle (vertical white arrows). (B) another small cystic lesion seen in the left upper abdomen (horizontal yellow arrow)
Figure 2: MRI abdomen and pelvic with contrast (A) Coronal T2-HASTE, (B) Coronal In phase T1-weighted images, (C) Coronal T1 post contrast, (D) Axial out phase T1-weighted images. Retroperitoneal large hemorrhagic lesions seen in the left lower abdomen (horizontal white arrows) and right psoas muscle (vertical white arrows). Not of internal nodule in image D. No enhancement in subtraction images (did not show).
Discussion
A complication of severe hemophilia when the regular factor activity in the human blood is below 1 % can cause hemophilic pseudotumor [1]. Hemophilic factor (AHF) deficiency is categorized into three categories: mild, moderate, and severe. The soft will indicate AHF greater than 5 %. The middle is between 1 -5 %, and the powerful are less than 1 % [6]. Diagnosing HP can be challenging. Also, the difficulty arises from needing more patient history. Missing the patient’s history, such as not knowing the patient’s hemophilia, makes the diagnosis more demanding. The difficulty comes because it is rare and the similarity to other disorders. In this case, the history of hemophilia is one of the essential clues to indicate a pseudotumor and AHF deficiency.
In addition, the MRI appearance with surrounded hemorrhage (Figure. 2) gives a significant clue to the radiologist to eliminate other indications such as hydatid cyst, which has an identical appearance to pseudotumor because hydatid cyst is rarely found with hemorrhage [8].
Conclusion
MRI and CT scans can be handy tools to diagnose HP. Additionally, investigating the patient history due to the similarity between HP and another similar cyst, such as hydatid cysts, can also be helpful.
Disclosure: No potential conflict of interest relevant to this article was reported.
The manuscript has been seen and approved by all authors
References
- Dupont MV, Coche EE (2015) CT and MRI Aspects of an Abdominal Hemophilic Pseudotumor. J Belg Soc Radiol. 99(2): 50-52.
- Jaovisidha S, Ryu KN, Hodler J, Schweitzer ME, Sartoris DJ, et al. (1997) Hemophilic pseudotumor: Spectrum of Mr Findings. Skeletal Radiology. 26(8): 468-474.
- Hermann G, Yeh HC, Gilbert, MS (1986) Computed tomography and ultrasonography of the hemophilic pseudotumor and their use in surgical planning. Skeletal Radiology. 15(2): 123-128.
- Sharma A, Lodhi JS, Lingaiah P, Kumar A, Arora S (2019) An Unusual Presentation of Hemophilia A: Pseudotumor of Distal End Radius-Masquerading as Giant Cell Tumor. J Hand Microsurgery. 11(Suppl 1): S11-S15.
- Liu S, Zhou X, Song A, Huo Z, Wang Y, et al. (2019) Successful treatment of giant abdominal hemophilic pseudotumors causing hydronephrosis. Postgraduate Medical Journal. 95(1130): 673- 674.
- García-Pérez R, Torres-Salmerón G, Sánchez-Bueno F, García- López A, Parrilla-Paricio P (2010) Intraabdominal hemophilic pseudotumor: Case report. Revista Española De Enfermedades Digestivas. 102(4): 275-80.
- Pedrosa I, Saíz A, Arrazola J, Ferreirós J, Pedrosa CS (2000) Hydatid disease: Radiologic and pathologic features and complications. Radiographics. 20(3): 795-817.
- Bächler P, Baladron MJ, Menias C, Beddings I, Loch R, et al. (2016) Multimodality imaging of liver infections: Differential diagnosis and potential pitfalls. RadioGraphics. 36(4): 1001-23.